Patient Story- Kasi: Endometriosis, Infertility and the Path to Motherhood
As Endometriosis Awareness Month comes to a close, we wanted to share Kasi’s journey. It’s one of strength, resilience and hope. Kasi endured years of pain from endometriosis, multiple surgeries and several IVF cycles. Through every challenge, she never gave up on her dream of becoming a mother. Today she holds that dream in her arms- her beautiful son, Koah.
He has brown russet-colored eyes that are full of depth. They sparkle when he laughs and when he looks at me. He has his father’s hair and my jawline. His latte-colored skin comes straight from me. He is the light of my life and for many dark years, I wondered if he’d ever be here.
Years of Pain Without Answers
I had a plan for my life as many women do. The plan was to finish graduate school, get married, buy a house, and then start a family. My early twenties had their own hardships that centered around midterms and quarter-life crises. I also had unusually painful periods that most doctors dismissed with instructions to start taking ibuprofen a couple days before my period would start. But the pain would still leave me curled in a ball in the middle of my bed every few months. A doctor at the health services recommended taking birth control pills to help regulate my periods and reduce the pain. It worked for several years. When my husband and I turned 30 years old, we decided that we wanted to start our family. That required me to stop taking the birth control pills and to begin planning the next part of our lives. We planned on 2 or 3 children. We talked about the types of parents we would be, and we made plans around their impending arrival. But the arrival seemed stalled.
The pain was back. Sometimes it would be debilitating, and it would cause me to miss work. I was also having digestive issues that would cause chronic constipation and discomfort. I started a new job that could be stressful, so I thought it was all stress related. In the winter of 2012, the holidays were rough. After Christmas, I found myself in significant pain. I recently switched doctors and decided to see my new doctor to find out what was going on.
The Diagnosis That Changed Everything
Dr. Melissa Kwak was the first doctor who listened to me when I told her about all the pain I was having. She ordered an MRI that started me on my journey. The MRI found a fibroid the size of a grapefruit on my uterus. She sent me for further testing with Dr. Brett Cassidy and he recommended that I have surgery to have the fibroid removed in February 2013. I was 32 years old. I remember feeling so frustrated that my body could betray me in that way. I know the depth of the betrayal.
The surgery was meant to be laparoscopic. They explained that I would have tiny keyhole incisions made in my abdomen and another in my belly button so that the machine could excise the fibroid without them having to open me up with a lateral incision. They expected everything to go easily and after recovery, we could begin trying to have a baby again. When I woke up from anesthesia, I was in overwhelming pain. I began screaming and the nurses rushed to me. I heard one say, “We need to manage her pain!” I knew immediately that something went wrong. I kept asking over and over what happened, but no one answered me.
“You have endometriosis,” my doctor later explained to me. They had to abandon the laparoscopic surgery as soon as they could see what they were dealing with. They had to open me up laterally (like a c-section). I had adhesions all over and this was the reason for my extreme pain during menstruation. With endometriosis, endometrial tissue is found in other areas of the pelvis. When the body menstruates, the tissue in these other areas, outside the uterus, bleed as well. The body treats these areas as internal bleeding and rushes to heal it and create scar tissue around it. These are called adhesions. My doctor was able to save my reproductive system and remove the adhesions. He gave us the green light to begin trying to have a baby again. He explained that being on birth control was unknowingly treating the endometriosis. But to start our family, I could not take medication for the condition. The instructions were to get pregnant fast since there was no cure for endometriosis and the adhesions can return. We were optimistic, but another year passed without a baby.
IVF and the Emotional Toll of Infertility
We realized that it was time to talk to a fertility specialist to assist us. Dr. Cassidy recommended that we see Dr. Charles Miller in Naperville, IL to assist us. However, our insurance didn’t cover Dr. Miler. So, in 2014 we began working with another fertility clinic. The doctor with this center, decided quickly that IVF would be the best option. We were 33 years old, so the odds were in our favor.
At this clinic, we ran into more complications. They had trouble with egg retrieval. They sent me back to Dr. Cassidy for another laparoscopic surgery to remove more endometrial adhesions. We finally got 10 embryos but only 4 survived. They transferred 2 embryos in December 2014. We would have to wait 2 weeks to find out if the embryos took and if we were going to be parents. During that 2-week wait, my father-in-law passed away from heart disease and we were mourning. I look back on that period with a lot of pain. I often wonder if the grief and the negative emotions I felt made my body inhospitable for those little babies. We found out that the embryos didn’t take a couple days before the funeral, so we grieved my husband’s father, and the loss of the embryos. I fell into a mild depression after that. I admitted this to my doctor, and she suggested that I begin seeing a therapist. I was dealing with a lot of guilt and grief over my father-in-law passing. I felt like I was selfish in his last days because I was so focused on the embryo transfer, but I also felt that I was a terrible mother to those embryos because I did not provide a positive environment where they could grow.
Infertility can be a lonely thing. Even though I was surrounded by doctors and nurses and friends and family who encouraged me, I still felt alone. I felt profound shame and inadequacy. I didn’t think that I was worthy to be a mother and maybe somehow God had ordained it to be this way. I received confirmation of my own perceived condemnation when a second embryo transfer did not yield a pregnancy. I needed time off. For a year, I didn’t want to think about fertility or trying to have a baby. But during this time off, the endometriosis did not leave me. The pain became severe again and I knew that I’d need to address it and decide if we’d want to try to be parents again. Through this time, we switched to a new insurance. I went to see Dr. Cassidy to ask about another surgery for the endometriosis. He asked us again if we thought about Dr. Charles Miller. He said he was one of the leading specialists in the area for endometriosis and he could do the surgery. We investigated our insurance coverage, and we were happy to find that Dr. Miller was covered.
Finding the Right Specialist
When we first met with Dr. Charles Miller, it was on a Sunday. He was dressed in a beautiful suit. He looked outstanding. He immediately helped us feel at ease. He tailored the treatment plan to me and my unique circumstances. That was refreshing, because our last doctor wanted to use the same protocol with me that she used for every woman she treated, regardless of the diagnosis. We were 35 years old and desperate to make things work. The fertility world talks about age 35 as the gateway into geriatric pregnancy. The percentages of successful live births begin to go down at this point and risks of birth defects and other issues increase. We were anxious to get started. I had 4 or 5 surgeries, numerous egg retrievals and 3 embryo transfers with Dr. Miller. I remember, after a disappointing cycle, we sat in Dr. Miller’s office with him. He was quiet after explaining what happened and we were quiet. I remember asking him not to give up on me. I remember he took my hand and told me that he was willing to fight along with us for as long as we were willing to fight.
In January 2020, I needed another surgery for endometriosis. I was 39 years old and desperate to try again before I turned 40. We had one frozen embryo left from the previous cycle. The plan was to have the surgery, do a few more egg retrievals so we could transfer more than one embryo. The odds are always better when you have more than one embryo to transfer. By the summer of 2020 I went for tests, that showed that I wasn’t ovulating after the last surgery and there wasn’t much hope of getting more embryos. Dr. Miller talked to us about donor eggs, but my husband and I didn’t want to give up on the dream of having a child that was a little bit of both of us. So, we decided to transfer the one embryo we had. We decided we were done with the whole IVF process. We started looking into foster care and adoption. It took another 6 months to get insurance and all other circumstances to line up.
One Last Chance at Motherhood
In February 2021, a few months after I turned 40-years-old, I came into the office to transfer the last embryo we had frozen. We were in the thick of COVID protocols so my husband couldn’t come in with me. When the doctor came in, I tearfully told him about the amazing impact he had on my life. I told him that no matter the outcome, I was just so grateful that I had the opportunity to reach for my dream when so many other women didn’t even get the chance to try. We both cried and he told me that he had a great feeling about that transfer. I had a sense of peace after that last cycle. In the past I did acupuncture after the embryo transfers to increase the odds of the embryo taking. But this last time, we chose to go to my father’s house and pray. My husband, my father, and I joined hands and prayed the most beautiful prayer about gratitude and joy regardless of the outcome.
The Call That Changed Everything
On the morning of my blood test after the 2-week-wait, I felt hopeful and peaceful. I knew this was going to be my last time going through the process and maybe knowing this gave me peace that day. Normally, the results of the pregnancy tests came to us on a portal app on my cell phone. I thought that I wouldn’t hear anything until the afternoon. During my morning break from work, I decided to lay down and take a nap. Before I could fall asleep, my phone started ringing and it was Dr. Miller’s office. They never called before on pregnancy test day, so my heart was in my throat when I answered the phone. The nurses in the office had me on speaker phone. The phlebotomist, the ultrasound tech, and two of the nurses were gathered around the phone. They asked me if I was sitting down. When I told them I was, one of the girls screamed, “You’re pregnant!” I immediately fell on my knees. I cried on the phone with them for what felt like an hour. I could hear a few ladies crying with me and I heard them yelling “Congratulations!’ I couldn’t even speak. It was 10 years of waiting. 10 years of crying. 10 years of wondering what I had done wrong, 10 years of disappointments. The emotion that flowed through my body in that moment was pure joy.
A Dream Come True
My pregnancy went forward without any complications. We were blessed because I was healthy, and the baby was healthy. I gave birth to a beautiful baby boy named Koah. I am certain that I just gazed at him for hours. I still love to look at him. We had waited so long for him, and he had waited for us as a frozen embryo. He was the very last to be transferred, but he was destined to make it into our arms. Koah is our only child, but our hearts remain open and excited about this beautiful life we will have with our son. I knew from the moment that my pregnancy was confirmed that I would share this story. I knew that I wanted to encourage other women who feel isolated while going through this journey. I persevered and I was able to experience the miracle of feeling a life growing inside me. I can watch him grow as a walking and breathing testament to my own strength and endurance. The journey taught me to feel worthy regardless of the outcome and I am looking forward to helping other women feel empowered and strong.
-Kasi
How Endometriosis Affects Fertility: Causes, Symptoms, Diagnosis and Treatment
We spoke with Dr. Laurence Jacobs, a reproductive endocrinologist with over 30 years of experience, to explore how endometriosis impacts fertility and how to recognize the signs of this often misunderstood condition.
How Does Endometriosis Affect Fertility?
Endometriosis can make it much more difficult to get pregnant. In fact, 20-50% of all infertile women have endometriosis, making it a prevalent issue in reproductive health.
One of the main ways endometriosis affects fertility is through scar tissue formation. When endometrial tissue grows outside the uterus, it can create scar tissue, adhesions and inflammation around the ovaries and fallopian tubes. This can often distort the normal anatomy of the pelvis, making it harder for the fallopian tubes to move over to the ovary and pick up the egg during ovulation.
Endometriosis can also interfere with ovulation. Endometriomas, which are cysts formed by endometriosis growing deep within the ovaries, can disrupt ovulation by affecting both the development and/or release of eggs. Additionally, some research suggests endometriosis can negatively affect the egg quality due to the inflammatory environment it creates within the pelvis.
Another concern is embryo implantation. The inflammation caused by the endometriosis can make it more difficult for the embryo to successfully implant within the uterine endometrial lining, leading to infertility or recurrent pregnancy loss.
The severity of endometriosis plays a significant role in its impact on fertility.
- Stages 3 or 4 (more advanced endometriosis) involve severe adhesions and endometriomas, which can have a major impact.
- Stages 1 or 2 (milder cases) may only involve small implants of endometriosis, which can still affect fertility but to a lesser degree.
The stage, severity and location of lesions and implants all play a significant role in how endometriosis affects fertility.
How Can You Tell If You Have Endometriosis?
The most common symptoms of endometriosis include:
- Pelvic pain
- Moderate to severe menstrual cramps
- Pain during sexual intercourse
Although some women with endometriosis have no symptoms at all. A pelvic exam can sometimes reveal signs of endometriosis, such as hard nodules at the bottom of the pelvis.
Ultrasound is another useful tool for identifying endometriosis. Endometriosis growing very deep inside the ovaries, can form a cyst called an endometrioma and these cysts can be seen on ultrasound. However, most smaller implants of endometriosis cannot be seen on ultrasound. Ultrasound can only detect advanced stage 3 or 4 endometriosis, while smaller implants and adhesions seen in Stage 1 or 2 may not be visible.
How Is Endometriosis Diagnosed?
Symptoms and signs of endometriosis and even ultrasounds can make one suspicious of endometriosis, but the only way to definitively diagnose the condition is through laparoscopy. A laparoscopy is a minimally invasive procedure that allows a surgeon to look inside the pelvis using a laparoscope, which is a thin, telescopic rod with a video camera on the end. Not only can laparoscopy surgery confirm endometriosis, but the procedure can treat it as well.
Why does surgical expertise matter?
Because advanced endometriosis (Stage 3 or 4) often involves severe adhesions affecting the ovaries, intestines, bladder and ureter, it is highly recommended that the laparoscopy be performed by a skilled reproductive surgeon rather than a general gynecologist.
- A skilled reproductive surgeon can both diagnose and remove endometriosis in one procedure.
- You don’t want to undergo surgery just for diagnosis, only to need a second procedure for treatment.
- A less experienced surgeon may leave some endometriosis behind or be unable to treat complex adhesions.
New Advances in Endometriosis Testing
In the last seven years, innovative diagnostic measures have been developed to help determine if a woman with no symptoms or ultrasound evidence might have endometriosis. It also helps physicians decide who would be a good candidate to undergo laparoscopy.
Back in the 1980s and 1990s, it was standard procedure that everyone with infertility undergo laparoscopy, but now we try to be much more selective. The ReceptivaDX test, an endometrial biopsy performed in the office, checking or sampling the uterine lining, measures a protein called BCL6, a marker usually associated with endometrial uterine inflammation and potentially silent endometriosis.
An abnormal biopsy result usually means there is endometriosis or inflammation in the pelvis. This biopsy can be very helpful for women who have no symptoms, evidence of endometriosis on ultrasound or unexplained fertility.
Seeking Expert Care
If you think you might have endometriosis, it is imperative to seek out an experienced reproductive surgeon specialized in treating advanced endometriosis. In my opinion, Dr. Charles Miller, Dr. Kirsten Sasaki, and Dr. Molly McKenna are among the best reproductive surgeons for endometriosis treatment in the Midwest. Their expertise ensures that patients receive the highest level of care for both diagnosis and treatment, improving their chances of achieving a successful pregnancy.
Request a consultation or call 630-428-2229 to schedule.
Welcome Dr. Laurence A. Jacobs
Dr. Laurence A. Jacobs is a Mayo Clinic fellowship-trained Reproductive Endocrinologist and Infertility Specialist (REI) in clinical practice in the Chicago area for over 45 years. With a commitment to providing compassionate, personalized care, Dr. Jacobs has helped thousands of infertile couples and individuals build their families through holistic and advanced fertility treatments. At CCRM Naperville/Charles E. Miller, MD & Associates, Dr. Jacobs performs new and existing Patient Consultations for general female infertility, male infertility, PCOS and IVF.
Dr. Jacobs earned his medical degree (M.D.) from Northwestern University where he later completed his 4-year residency in Obstetrics and Gynecology. Dr. Jacobs is board certified in OB/Gyn and practiced as a general OB/Gyn for 7 years. Then he further specialized in Reproductive Endocrinology and Infertility (REI), successfully completing his fellowship training at the prestigious Mayo Clinic. Over the course of his distinguished career, Dr. Jacobs has held academic and clinical leadership roles, authored many peer-reviewed publications, and presented at national conferences on infertility treatment innovations.
After completing his REI Fellowship at the Mayo Clinic, Dr. Jacobs initially joined Dr. Charles E. Miller as a Partner, practicing Infertility and IVF for 7 years together until 1995. Subsequently, he became a Partner at Fertility Centers of IL for well over 20 years until his mandatory retirement. He has now re-joined his friend and colleague, Dr. Charles E. Miller, bringing his wealth of knowledge and clinical ability to CCRM- Naperville. Dr. Jacobs is honored to be a part of the highly acclaimed CCRM (Colorado Center for Reproductive Medicine) network. For many decades, CCRM, a leader in exceptional cutting-edge fertility care, genetics and research, has continuously produced some of the highest IVF live birth rates in the U.S.
Nationally recognized for his patient-centered approach, Dr. Jacobs focuses on understanding each patient’s unique fertility challenges. His deep expertise in diagnostics, IVF and personalized care plans makes him highly sought-after for New Patient Consultations. He is particularly passionate about helping patients with unexplained infertility, ovulation disorders, recurrent pregnancy loss, PCOS, elective Egg vitrification (Cryopreservation), and does comprehensive consultations for those seeking second opinions, especially for failed IVF.
“As your doctor, I am committed to compassionate and respectful care. The measure of an excellent ‘fertility specialist’ should not be based solely on pregnancy rates, but also on how patients feel about the care they receive. Most of my patients are referred to me by ‘word of mouth’ from physicians and patients, as well as internet reviews. I get tremendous satisfaction from what I do, and what I do every day makes a difference in people's lives. I take that responsibility very seriously.”
AWARDS & HONORS
Dr. Jacobs has received many awards for his contributions to reproductive medicine. He has been repeatedly honored by distinguished recognition as a Top Infertility Doctor by Castle Connolly publications, AMERICA’S TOP DOCTORS (top 1% of Infertility MDs Nationwide) for over 20 consecutive years. CHICAGO Magazine has repeatedly selected Dr. Jacobs as a ‘Top Doctor Chicago Area’ for Infertility. He is a Five-Star Physician on Healthgrades. Dr. Jacobs is well-known for his kindness, empathy, quick wit, and sense of humor which puts his patients at ease. He “listens and spends time” and accordingly has often been honored with Vitals.com’s Compassionate Doctor Award, recognizing exceptional care and grace based on patient reviews.
He is also actively involved in professional organizations such as the American Society for Reproductive Medicine (ASRM) and is a Fellow, American College Obstetrics & Gynecology.
When not practicing medicine, Dr. Jacobs enjoys spending time with his wife, Diana, doing boating, gardening, Netflix, and riding their Vespas together in the countryside. They also love traveling and visiting their adult children and grandchildren.
Understanding Male Factor Infertility- Semen Analysis
Did you know that male factor infertility accounts for almost half of all infertility cases? It’s a common issue that many men face, but it's not talked about as often as female infertility.
As part of a comprehensive approach, we order a semen analysis for every male partner after taking a thorough medical history review.
What is a Semen Analysis?
A semen analysis is a lab test that evaluates male fertility. The test is usually done by having the partner collect a masturbated sample after abstaining from intercourse for 3-7 days. The sample is ejaculated into a sterile container, usually a sterile wide-mouth urine cup, either at home or in the office. The analysis evaluates:
- Specimen Volume
- Sperm Concentration
- Total Sperm Count
- Motility
- Morphology
Semen Analysis Metrics
Specimen Volume
Specimen Volume refers to the amount of semen produced.
Usual Parameter: 1.5 ml or greater
Sperm Concentration
Sperm Concentration measures the density of sperm within a given volume of semen.
Usual Parameter: Greater than or equal to 15 x 106 spermatozoa
Sperm Count
Usual Parameter: Between 20-100 million sperm.
Generally, anything below 20 million is considered a low sperm count. However, sperm numbers can change daily, weekly and monthly. Colds, flus, STDs, infections, antibiotics, temperature and ejaculation frequencies will affect the number. Men with sperm counts of well below 20 million have often been able to father children.
Morphology
Morphology is the shape of the sperm. Abnormally shaped sperm appear with malformed heads (two heads, tiny heads, round heads) and tails (two tails, short tails). These shapes tend to affect their motility.
Usual Parameter: Anything greater than or equal to 4% normally shaped sperm indicates good morphology based off Krueger Strict criteria.
Motility
Motility is the ability of sperm to move forward by swimming inside the vagina, through the cervix, and into the fallopian tubes, where it could fertilize an egg.
Usual Parameter: More than 40% motile
Next Steps After Semen Analysis
After conducting a semen analysis, Dr. Miller carefully reviews the results and recommends the best next steps for the couple. Depending on the findings, this may involve treatments such as intrauterine insemination (IUI), in vitro fertilization (IVF), or the use of donor sperm. Each treatment plan is tailored to address the specific needs and challenges identified during the analysis.
Whether you are with a partner or are ready to move ahead on your own, schedule an initial consultation with us today and learn more
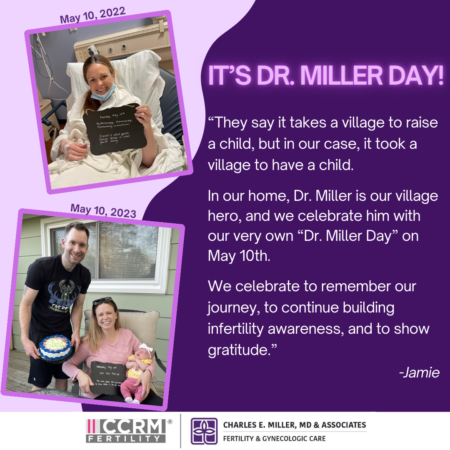
May 10 is Dr. Miller Day!
Did you know May 10th is Dr. Miller Day? Neither did we, until our patient, Jamie, shared that she created this special day to remember her fertility journey, the support she received from her “village” and of course the doctor who helped her become a mom!
Jamie writes:
Our fertility journey started as most do, with a lot of hope and a lot of disappointing negative pregnancy tests. During my initial testing, I found out I had 2 fibroids and one was very large. Although I kept asking about the large one, I was told by 3 different doctors that they weren’t an issue and was encouraged to start IUI or IVF.
Although reluctant, we started planning on how and when to move forward. Through that process, we started applying for grants. While looking at the grant application, I started reading into how it would be scored. In the fine print, I noticed certain types of fibroids would disqualify us from the grant, and that is because they can make IVF less successful. This made me, once again, question my fibroid. I told my husband that I wanted to find an expert opinion to rule out the fibroid causing my fertility issues before beginning any treatment. I started to research fibroid experts, and one name kept coming up again and again in my search, Dr. Charles Miller.
In April 2022, during my consultation with Dr. Miller, I expected to hear, once again, that the fibroid was “fine.” Dr. Miller recommended surgery, and on May 10th, 2022 he successfully removed both fibroids. We spent the next few months healing, trying to enjoy life, appreciating what we have, and planning our next steps to bring home a baby of our own.
In August 2022, I returned to Dr. Miller’s office, and he told me that things healed well and we could start trying again. During that same month, I was on pins and needles hoping to hear that we got the IVF cycle grant. However, less than three weeks after my follow-up visit with Dr. Miller, our jaws dropped when we got our positive pregnancy test! It was clear that the fibroid was what had been causing my infertility, and if we hadn’t done our research and sought out Dr. Miller’s expertise, we would have spent thousands on IVF without any success.
On April 17, 2023 our miracle baby girl, Fontana, was delivered via c-section. We cannot thank Dr. Miller enough for taking his time to listen to our concerns, truly evaluating the fibroid and its impact, and for his flawless surgery. Without Dr. Miller, we wouldn’t have had a first birthday to celebrate last month.
This Friday we will celebrate our second Dr. Miller Day. This year we took the time to reflect and appreciate those who were a part of our village by writing cards to family, friends, and those strangers who supported us during our darkest days of infertility. Each person is represented by a house, and when we put them all together, it was empowering to see just how many people helped us along the way. No two infertility journeys are the same, but for those still in the trenches, trust your gut and advocate for yourself.
Patient Story- SJ
SJ has been a patient of ours since 2012. After years of trying at another clinic, she underwent surgery with Dr. Miller, and then made the difficult decision to use donor eggs. In 2013, SJ and her husband welcomed twins! However, their family was not complete, and they welcomed another son last year! SJ understands the complexities of using donor eggs but hopes her journey brings awareness and inspiration to others in similar situations.
If you would like to learn more about our donor egg program, please contact Lindsey Bartscher (lbartscher at drcharlesmiller.com). Special thanks to SJ and her husband for sharing their inspiring story.

Our journey to build our family was a long one, but we are happy to say we are on the "other side" of infertility thanks to Dr. Miller and his wonderful staff!
We started trying to conceive in May 2009 when I was 29 years old. Both of our parents had conceived easily, and we were both healthy, so we didn't expect to have any problems. Unfortunately, after a year of negative cycles, we started seeing a fertility doctor in June 2010. Despite all our tests looking normal, we did four IUIs that all failed. When we finally got to the point of doing IVF, we just expected it would work. Our first IVF cycle, I got pregnant and for the first time ever saw two pink lines! Even though my hcg numbers were low, I thought just the fact that I'd finally seen a positive pregnancy test meant things might work out. We lost the pregnancy around 5.5 weeks and quickly moved into a frozen embryo transfer (FET). That cycle failed, and we did two more IVF retrieval cycles and fresh transfers that both failed. After our third failed IVF cycle, my original fertility doctor suggested that we may need to use donor eggs. I was not ready to move forward with donor eggs then, so we tried one more IVF cycle with our original doctor. When that cycle failed, our doctor suggested not only donor eggs but donor sperm. We asked our doctor if he would be willing to perform further testing and a laparoscopy to test for endometriosis, since my sister had recently been diagnosed with it. When he refused, we decided it was time to switch clinics.
I had a friend who was able to get pregnant after a procedure Dr. Miller performed, so based on her recommendation and a lot of research, we decided Dr. Miller's office was the right place for us to continue our journey. Dr. Miller was completely on the same page as us and understood that before we did donor eggs or donor sperm or another IVF, we wanted to be 100% sure we had tested for any potential issues like endometriosis or immune issues that could affect implantation of an embryo. Our motto was "no regrets," so we wanted to make sure we had no regrets about our decisions on this fertility journey. Dr. Miller performed a laparoscopy after finding mild endometriosis, and he discovered I had homozygous MTHFR, both issues he thought could affect IVF success. We tried one more IUI cycle and one IVF cycle with Dr. Miller. After our first IVF cycle with Dr. Miller, he told me I had "soft" eggs and recommended donor eggs. He said he did not think we needed donor sperm, but he showed us the statistics on donor eggs and explained how such a cycle would work. Dr. Miller's Donor Egg IVF Coordinator also gave us a lot of information on donor egg agencies and counselors.
After taking a few months to regroup and make sure we were ready, we decided to move forward with donor eggs in August 2012. Dr. Miller also added Lovenox and Medrol to my cycle due to my MTHFR and repeated IVF failures. We found an amazing donor egg agency (Graceful Conceptions) and moved forward with a fresh donor egg cycle in December 2012. The difference between our donor egg cycle and my egg cycles was night and day! We had so many more embryos to work with that we did with my cycles, and they were all top quality! We transferred two embryos on December 18th and were able to freeze five more high graded embryos. And right before Christmas I got two beautiful pink lines on a pregnancy test! It was the BEST Christmas gift we could ever imagine! We found out two weeks later that we were expecting not only one but TWO babies!
Our twins were born healthy in 2013, and we kept our frozen embryos for several years. Eventually, in 2022, we decided to try and expand our family. We knew it might take a few tries, but we got lucky and had success on our second frozen embryo transfer in May 2022.
We know some people are not comfortable with donor eggs, but Dr. Miller made us feel so comfortable about it, and he reminded me that with donor eggs I would still be carrying my children. We know our three beautiful children would never have been possible without donor eggs or Dr. Miller. We are forever grateful we decided to switch clinics back in 2012, and we are thankful Dr. Miller was so straightforward about donor eggs being our best chance of having a baby and building our family. We explained to our kids that donor eggs are just part of their story and something that makes them special, and they will always know how much they were wanted and loved! We hope our story gives other couples hope, especially when faced with failed IVF cycles. "Success" looks different for everyone, but we are blessed and grateful that our donor, Dr. Miller and science have made our family possible!
-SJ
Ovarian Pexy- A Simple Procedure to Help Improve Egg Retrieval Outcomes
We posted a video of Dr. Miller discussing a recent surgical procedure he performed called an Ovarian Pexy that helps improve egg retrieval outcomes. We figured this was a procedure many were unfamiliar with, so we asked Dr. Miller for more information. Get ready to understand how this simple procedure can make a big difference on your road to becoming a parent.
Q: What is an Ovarian Pexy?
Dr. Miller: A laparoscopic procedure to move the ovaries closer into the pelvis so that the follicles can be more easily identifiable.
Q: How do you know if you are a good candidate for Ovarian Pexy?
Dr. Miller: The procedure would be performed on someone whose ovaries are out of position. A woman can be born with her ovaries misplaced, making IVF difficult. Additionally, another potential cause is adhesive disease – whether from infection, endometriosis or prior surgery, the ovaries are simply pulled away from the pelvis.
However, keep in mind that you don’t know whether or not there is room for improvement until you look at the anatomy. If I cannot see the ovary, I will not take the patient to stimulation. Generally, we have indications that the ovary is not in the right place and see this while the patient is undergoing transvaginal ultrasound or when I perform a saline infused sonogram. At that point, I recommend surgery. Pexy of the ovaries is ultimately a game time decision at the time of surgery, when the anatomy can be seen.
Q: Why does this procedure improve your chances for a more successful egg retrieval?
Dr. Miller: It gets the ovaries to a place where they can be easily visualized via ultrasound and thus, makes egg retrieval easier.
Q: What is the recovery time and how soon can you do an egg retrieval after the procedure?
Dr. Miller: The recovery time is 5-7 days at home and the patient can start preparing for an egg retrieval with her next cycle.
Q: How common is an Ovarian Pexy?
Dr. Miller: Since most reproductive endocrinologists do not perform surgery, this procedure is not routinely performed. Instead, patients settle for a lesser amount of eggs. Oftentimes, Dr. Miller sees patients who have gone through cycles with other physicians and have not had eggs retrieved on one side because of the ovary position. After the ovarian pexy procedure, patients can go from not being able to retrieve eggs to having a comparable number of eggs retrieved from either ovary.
Interested in scheduling a consultation with Dr. Miller? Call 630-428-2229 to set up an appointment or request a consultation online.
IVF Superstitions Uncovered: From McDonald’s French Fries to Pineapples and More
You’ve been there, late night scrolling through Instagram or TikTok and filing away any and all tricks that hold the key to a successful embryo transfer. We decided to take a closer look at some of these IVF superstitions and better understand their origins.
McDonald’s French Fries
One popular superstition among IVF patients is consuming McDonald’s French Fries on the way home from the embryo transfer. The origin of this myth is unclear, but it is believed that the high salt content in the fries may help the body to absorb any excess fluids, potentially fending off ovarian hyperstimulation syndrome (OHSS). However, it should be noted that there is no scientific evidence to support this belief.
Pineapple
Eating one ring of pineapple, including the core, daily for five days starting on the day of the embryo transfer is another common IVF superstition. Because pineapple contains bromelain, a mix of enzymes that may break down scar tissue and decrease inflammation, patients were eating pineapple on an empty stomach the day of their embryo transfer. But again, there is no scientific research that supports this will improve implantation.
Pomegranate Juice
Drinking pomegranate juice before and after the embryo transfer is another IVF superstition. Pomegranate juice is known to contain antioxidants and vitamins, and it is thought to thicken the uterine lining, which could aid with implantation. Additionally, the antioxidants may improve egg quality prior to the transfer. Despite these potential benefits, there’s no scientific evidence to back up this practice.
Water
Drinking more than 64 ounces of water in the days after the embryo transfer is another common recommendation. It is believed that staying well-hydrated can support blood flow to the uterus, which in turn can aid in implantation.
Warm Feet/Cozy Socks
Many people believe that keeping your feet warm during the transfer is beneficial. The reasoning is that if your body is sending blood flow to your extremities to keep your feet warm, it may redirect blood flow away from the uterus and embryo. However, like all the other superstitions, the scientific support for this is lacking.
Dr. Charles Miller Weighs in on IVF Superstitions
Dr. Miller, a renowned fertility expert, acknowledges the existence of these superstitions. He notes, “While all of these IVF myths have some sort of scientific support, at the end of the day, none of them have been studied and certainly, none have been shown to be effective.”
He adds humorously, “Nonetheless, I’m waiting for the day that one of our patients walks into the office eating the McDonald‘s Infertility Happy Meal consisting of fries, pineapple core and pomegranate juice. I guess it’s healthier than chicken nuggets and a Coke!”
In conclusion, while these IVF superstitions may seem to have a scientific basis, there is no evidence to suggest that any of them actually influence the outcomes of IVF treatment and they should not replace the medical advice from your fertility care team. Remember, success in IVF is primarily determined by medical factors and a tailored treatment plan.
The Advanced IVF Institute Joins the CCRM Fertility Network of Clinics

Big news for our practice- the best just got better! We are pleased to announce we are now a part of the CCRM Fertility network of clinics. CCRM Fertility is a global pioneer in fertility treatment, research and science and specializes in the most advanced fertility treatments, with deep expertise in IVF, fertility testing, egg freezing, preimplantation genetic testing, third party reproduction and egg donation, achieving some of the highest Iive birth success rates in the U.S.
Dr. Miller and our dedicated and innovative team can’t wait to join forces with CCRM Fertility to provide exceptional care to our patients and give them the best opportunity for success.
Rest assured, Dr. Miller will remain as Practice Director and you will continue to receive the outstanding and personalized care you expect of us; however, now your access to top-tier medical resources has expanded to become even more innovative, efficient and accessible.
Dr. Miller had this to say: “It is an honor to join the prestigious CCRM Fertility network. Together, we are committed to our patients through innovative thought, procedures and technologies. I look forward to caring for existing patients and welcoming new patients through our doors as they face fertility and gynecologic challenges.”
We are excited to join with CCRM Fertility to bring joy to even more families! Check out the official press release below.
CCRM Fertility Broadens North American Footprint By Adding The Advanced IVF Institute to its Network
CHICAGO, Aug. 2, 2023 /PRNewswire/ -- CCRM Fertility, a global pioneer in fertility treatment, research and science, has added The Advanced IVF Institute, to its rapidly expanding fertility treatment and family-building network. Dr. Charles Miller leads two Chicago-area locations and provides cutting-edge fertility treatments, including in vitro fertilization (IVF), fertility preservation and reproductive surgery.
For more than 35 years, CCRM Fertility has helped transform lives through exceptional fertility care. CCRM Fertility's diverse, highly regarded team of physicians, research scientists, embryologists and professional staff are dedicated to helping patients achieve their dream of having a baby today, or in the future, achieving some of the highest Iive-birth success rates in the U.S. CCRM Fertility's expansive network currently serves 16 major metropolitan areas with 37 locations across the U.S. and Canada. Now, Chicagoans can have the benefit of the CCRM expertise in their own backyard.
"We are excited to welcome Dr. Miller and his team to our network, as they spearhead one of Chicago's leading IVF and surgery clinics and are recognized nationally and globally," said CCRM Fertility CEO Bob LaGalia. "Dr. Miller is an innovator in reproductive surgery and has a passion for learning new procedures, techniques and instrumentation that can positively impact patient outcomes. Dr. Miller and his experienced team will be an invaluable asset to CCRM as we collaborate to make assisted reproductive technologies more efficient and accessible for our patients."
As an internationally renowned expert in minimally invasive gynecologic surgery and in the treatment of infertility, Dr. Miller founded The Advanced IVF Institute in 2008. He is a graduate of the Honors Program in Medical Education from Northwestern University and completed his residency in obstetrics and gynecology at the University of Texas Southwestern Medical School, Parkland Memorial Hospital. Dr. Miller then earned his fellowship in reproductive endocrinology and infertility at the Hospital of the University of Pennsylvania.
Dr. Miller is a past president (2008) of the AAGL (formerly the American Association of Gynecologic Laparoscopists), the largest association of laparoscopic and hysteroscopic surgeons dedicated to the research and advancement of minimally invasive gynecologic procedures. Dr. Miller is also a past president (2011-2013) of the ISGE (International Society for Gynecologic Endoscopy).
In 2022, Dr. Miller received the AAGL esteemed distinction of Honorary Chair for his exemplary service to the AAGL and the outstanding contributions he has made in the field of reproductive medicine and minimally invasive gynecologic surgery.
Dr. Miller is the Director of Minimally Invasive Gynecologic Surgery and since 2010, Director of the Fellowship in Minimally Invasive Gynecologic Surgery Program at Advocate Lutheran General Hospital. He is the current president of the Foundation of the AAGL. He is also a faculty member of the Clinical Fellowship in Reproductive Medicine and Immunology, Rosalind Franklin University of Medicine and Science. Dr. Miller's ongoing dedication to developing young minimally invasive gynecologic surgeons earned him the AAGL's honorable John F. Steege, MD, Mentorship Award in 2018.
"It is an honor to join the prestigious CCRM Fertility network. Together, we are committed to our patients through innovative thought, procedures, and technologies," said Dr. Miller, who will continue to serve as Practice Director. "I look forward to caring for existing patients and welcoming new patients through our doors as they face fertility and gynecologic challenges."
About CCRM Fertility
CCRM Fertility is a global pioneer in fertility treatment, research and science. Founded by Dr. William Schoolcraft more than 35 years ago, CCRM Fertility specializes in the most advanced fertility treatments, with deep expertise in IVF, fertility testing, egg freezing, preimplantation genetic testing, third party reproduction and egg donation. CCRM Fertility leverages its own data and a dedicated team of in-house reproductive endocrinologists, embryologists and geneticists to deliver industry-leading outcomes. CCRM Fertility is a proud strategic partner of Unified Women's Healthcare, which is accelerating meaningful change in women's healthcare by building healthy, innovative and mission-driven businesses to meet the comprehensive needs of women across the entirety of their health journey. For more information, visit www.ccrmivf.com.
IVF Patient Journey- Karen

“I took time to educate myself about the IVF process. I started following some fertility accounts on Instagram and realized how big this community is. It’s the worst club to be a part of, but it has the best members!”
Today we are excited to introduce a new type of patient story to you. We will be sharing Karen’s journey and her efforts to become a mother. Karen had no reason to suspect she would have trouble conceiving until she tried for almost a year with no success. Now she is preparing to go through IVF and is ready to share the good, bad and the emotional with you. It is important to remember that each patient case is unique and Dr. Miller personalizes each treatment plan based on the patient’s age, medical history and test results. Here is Karen’s story:
My name is Karen and I am 38 years old, I have been married to my husband for four years and we live in Lombard with our sweet 5-year-old boxer mix, Cali. When my husband and I started trying for a family in 2021 and it wasn’t happening as quickly as I thought, I got worried. We both live a very healthy lifestyle, have clean bills of health and never thought we would have any issues trying to conceive. I had a ton of girlfriends that got pregnant very quickly, but then I also had several that went through IVF or were currently going through it. I didn’t know much about IVF because I tried not to let my mind think that would ever be an option for us. But then reality started to hit me. After eight months of no success, we decided that we needed to look into the IVF process and find a doctor.
I found Dr. Miller by doing some research on local doctors online through RE doctor websites. My friends who went through IVF all had different stories and different outcomes, with doctors all over the suburbs. My main concern was finding a clinic that didn’t make me feel like just a number. I wanted a doctor that had years of experience, would take the time to understand what we were going through and not push us through the consultation process. I also wanted to make sure there was a supportive nursing team that would be there for us during our journey. After our first meeting with Dr. Miller, I said to my husband, “Wow, this man is going to help get us our baby, I like him!”
After all the bloodwork, baseline ultrasound, HSN and semen analysis, we found out that my husband and I are both factors. Obviously my age was a huge factor and my husband had abnormal morphology, which made Dr. Miller suggest that we should go straight to IVF with ICSI (a method that involves injecting sperm directly into an egg to induce fertilization and pregnancy).
Actually hearing those words brought me to tears after we got off the call. I couldn’t believe we were going to have to go through this. A ton of questions went through my mind of why can’t I just be like everyone else, why can’t this be easy for us? I took time to educate myself about the IVF process. I started following some fertility accounts on Instagram and realized how big this community is. It’s the worst club to be a part of, but it has the best members! Finding girls that are currently going through the exact same process is a blessing. They totally know what you are going through and they feel your pains, the struggles and the wins.
Fast forward to October of 2022, and we were ready for our first round for egg retrieval. I started stims and was on a very basic protocol- menopur, follistim, ganirelix and double trigger shot. Once I got that big box of meds delivered, I was a little overwhelmed. Organizing, setting up my area where I was going to do the shots and going through the consultation with Nurse Patty, gave me the confidence that I was ready to take on the shots. I watched a ton of videos online of girls that were going through stims on Instagram to hype me up.
I had talked about the shots with my husband and showed him videos to get him ready for what I was going to be doing. I asked him (even though I knew I was going to be giving myself the shots) if he wanted to give me the shots and he said he would do them if I didn’t think I could. I let him know that he was off the hook with the stim shots, but that he would have to step up to give me the PIO shots once we got to that point in our journey.
To be honest, the shots were not that bad. Mixing and getting the shots prepped is the most hassle. I usually put on some music to sing along to as I am doing the shots to take my mind off what is going on!
I did ten days of shots and had my egg retrieval on November 3. I got six eggs! It was one more than I thought I was going to get. Results came the next day, that four matured and two fertilized with ICSI. Then we waited six more days to hear how those two did. On day 6, we received a message that only one made it to blast and a biopsy was being sent off for PGT-A testing.
We went through another long two week wait. I received the result that our only embryo was low mosaic- trisomy 1. It was heartbreaking to hear that our only embryo from our first egg retrieval had these results. We didn’t really understand what this meant, so we scheduled a follow up call with Igenomix with a genetic counselor to review the results. I am so glad we did, because after finding out what low mosaic really meant, we decided that we indeed were going to keep this embryo frozen. There might be some hope with this little embaby. After processing all this news, we knew that we had to get right back into another egg retrieval. When we first started this process, we were prepared with the possibility that we were going to have to do multiple egg retrievals based off of my test results.
At the end of November, we had our follow up consultation with Dr. Miller to review what happened and get his thoughts. He told us that this next round was going to be different and we are going to switch up the protocol now that we know what worked and what didn’t work. He gave us so much hope during that call, making sure to remind us that we are going to get our baby! Since I knew we would be starting the process again sometime in January, my husband and I just took the time to enjoy the holidays and not focus on IVF. It was a nice distraction.
Heading into round 2, I am excited and nervous. I am looking forward to seeing the end results with this retrieval since we are switching up my protocol. Even though I have been through this process once and I know what to expect, I have a feeling this path will be different and that’s ok. The main thing is that I have my support group to cheer me on, sending me positive vibes and prayers. Here we go round 2!
Stay tuned to follow Karen’s journey as she prepares for her second egg retrieval . She is excited to share her story with you and shed some light into the IVF process.