Patient Story- Rachael

“Our plan was always to have a baby, but our path certainly wasn’t a straight line.”
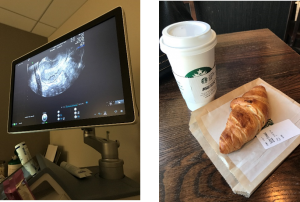
Our next patient story is from Rachael. Rachael’s journey to motherhood has not been an easy one. After undergoing several unsuccessful rounds of IVF, Dr. Miller advised Rachel to consider using an egg donor. In her story, Rachel describes the process she and her husband went through to choose an egg donor and what advice they would give to others in her situation. Rachael’s story has a happy ending- she is now pregnant and due with a baby boy in February!
Rachael writes:
To say that our journey was a difficult one is an understatement.
I was 34 years old when we wanted to start our family. After six months of trying on our own, we met with Dr. Miller. Testing and medication followed, and we eventually discovered – after finding out I had a diminished ovarian reserve, as well as confirming that I had a unicornuate uterus – that IVF was a route we needed to take. We diligently went to work ordering medication, setting up appointments, and saying so many prayers. Unfortunately, our first round failed. We just kept thinking, “This is it!” only to find ourselves back at square one.
When I met with Dr. Miller for our follow-up consult, he had another plan to try again. Upon leaving our meeting, he told me, “Stick with me, Rach! Rome wasn’t built in a day.” Knowing this was true, and knowing we had faith in our doctor, we trudged ahead and kept going. What followed were an additional five rounds (some stopped before retrieval), further testing and added medication, laparoscopic surgery, and the need to put on more weight in hopes that it would help my egg quality.
After several additional rounds of IVF and additional embryos from said rounds that didn’t take, our insurance plan was running out of options for us to keep moving forward. Dr. Miller advised us not to do the egg retrieval with my own eggs at that point and suggested turning to an egg donor. We were absolutely heartbroken. We knew that this was a real possibility, but the news was hard to take in. We were at the end of stimulation injections, and my body just wasn’t cooperating (which had happened during another of our previous cycles). Knowing my track record, Dr. Miller was concerned that this round would not work and then we’d really be out of options with my insurance. We converted the round to an IUI, but it didn’t take. A month later we transferred the one frozen embryo we had (insurance would still cover that), but we were left with a negative result.
We were angry, frustrated, and beyond depressed. We knew it was no one’s fault (I had to keep reminding myself that I did nothing wrong), but we couldn’t understand why it was happening. We did absolutely everything we possibly could to have a positive outcome, but were left with nothing but grief. You know everyone means well when they offer their condolences, but there are times when IVF is an incredibly isolating experience.
A few months later, we met with Dr. Miller again to discuss using an egg donor. He answered all our questions and felt optimistic about this new plan. When we were ready, we contacted an agency to get information. Later that fall, we chose our egg donor and started to feel more optimistic ourselves. Our donor went through the testing process and started some medication. We had psychological evaluations to make sure that everyone was in the right state of mind to go through this process, and we met with a lawyer to go through the contingencies of everything.
Our donor finally had her egg retrieval in February; we received 48 eggs (which was incredible!), and out of the 48, we had 17 embryos to freeze. We couldn’t quite sync up cycles, so we worked toward an April transfer, but then that got canceled due to me catching COVID-19. We were finally able to complete our transfer in May, and at the end of the month we received our first positive pregnancy test! I’m due in early February with a boy and am currently 18 weeks along (for a frame of reference, I am now 39 years old).
Moving forward, we have 16 embryos at our disposal. Besides some days where I didn’t feel great in the first trimester, my energy has bounced back in the second trimester and I feel pretty good! We’re really looking forward to the future and still cannot believe that we’re on the other side after years of wondering “what if?”
It was a long, difficult four-and-a-half years to get to this point. There were so many tears, early morning appointments, and hours upon hours of frustrating phone calls with insurance and pharmaceutical companies. There were so many pregnancy announcements by friends and family. There were so many times when we felt raw, numb, and alone. But on the other hand, we had hope. We had a strong support system, and we had a caring doctor who genuinely wanted the best for us. Dr. Miller’s staff was so kind and offered me hugs on more than one occasion when we received bad news. We learned to give into the unknown (something difficult for us teachers to do) and trust that we were doing everything we could.
If I can offer advice, I’d stress the importance of learning to pivot. Our plan was always to have a baby, but our path certainly wasn’t a straight line. We had to adjust the details of our dream, but that doesn’t mean that we’ll be any less of parents than we would have if things had worked with my genetics. Our dream could still be a reality, but adjustments were needed. Keep the end goal in mind: if it’s to have a child, understand that what that means might look different than what you anticipated when you started the journey.
If you find yourself in need of an egg donor (or sperm donor, if that’s the issue), I’d encourage you to take your time and go through the process when you’re ready. Don’t try to look for yourself in the pool of applicants; you won’t be there, and that’s okay. When we first got information from the egg donor agency, they encouraged us to not pay as much attention to pictures, but to focus on the information: we examined their health history and that of their relatives; we listened to their reasons for being a donor; we screened applications for the possibility of twins and triplets (given my unicornuate uterus, multiple births at one time was not considered a viable option); we also poured over their previous donor cycles to see what kind of success they had.
In the end, we chose someone who looked happy. She genuinely wanted to help other people conceive and assisted others in that goal already. The agency (and Dr. Miller’s office) couldn’t say enough good things about her, which was really reassuring. Besides matching my ethnicity, she does not look like me, but I’m keeping in mind that our boy very well may look more like my husband than the donor. If he doesn’t, that’s okay, too. This was something I had to learn to get comfortable with before we officially went through the donation process.
There are times when I look back at the last few years and the pain comes crashing back, and I’d be lying if I said it was easy to move on from my genetics. However, at the end of the day, the goal is to have a baby, and I learned that it is still possible if my genetics are no longer an option. This could be a path for you, too.
We would also encourage you to let people in and have a support network. My husband and I did not always want to talk about our struggles, but knowing we could speak with family and friends was helpful (and there are other support groups if you aren’t getting the support you need from those around you, too). Even though most of the people you know might not “get” the struggle you’re going through, it’s important to remember how many people are in your corner. You’re going to feel alone. You’re not.
Keep the faith. We’re rooting for you!
Patient Story- Courtney

“Keep going even when it feels like you can’t… The little victories will give you strength.”
Today’s patient story is from Courtney. Courtney discovered she had endometriosis when she and her husband were not able to conceive naturally after several months of trying. After undergoing surgery with Dr. Miller, she was able to get pregnant via IVF and just welcomed a baby boy only three weeks ago! Congratulations Courtney!
Courtney writes:
My husband and I began trying to conceive in late 2017. While at my yearly gyno appointment in May 2018, I mentioned we were trying to conceive. I was told to track ovulation with an app and/or pee sticks and go from there. My period had always been like clockwork and I learned that my ovulation was too. I maybe had heavier/more painful periods but nothing that ibuprofen and a heating pad couldn’t fix. My gynecologist did an internal ultrasound and noticed that one ovary was dense, leading her to believe that I might not ovulate on that side, however my pee sticks indicated that I did.
We ended up getting pregnant on our own in the summer of 2019, but that ended in a miscarriage (D&C) as there was nothing in the sac. I then had the dye test to see if my tubes were blocked and they were not. I also did 3 rounds of clomid with no pregnancy. This was the end of the road with my regular gynecologist as she couldn’t help me any further.
I then went to another gynecologist in my hometown to move onto IUIs. He did a natural IUI with no luck. Then we tried a medicated (clomid) IUI with no luck either. During this process, he did an internal ultrasound and that’s when I first learned I possibly had endometriosis. He referred me to Dr Miller.
I had laparoscopic surgery with Dr. Miller in Feb 2021 for endometriosis. We decided to try surgery before an egg retrieval, because Dr. Miller thought he could clean me out and then we could try to conceive naturally or with clomid as he didn’t think the endometriosis was as bad as it turned out to be. However, during surgery he found stage 4 endometriosis on my ovaries and appendix. He removed my appendix and did what he could on my ovaries in order to preserve them for IVF.
After my surgery, Dr Miller said that the endometriosis had been there for quite awhile because the cysts were so fixed to my ovaries. He said he did what he could to minimize the cysts but he couldn’t get rid of them fully because that would ruin good ovarian tissue for IVF. After I’m done having kids, I can have another surgery to fully clean me out.
It was invaluable to have Dr. Miller as my surgeon and fertility specialist. The entire time he was focused on the goal at hand- to have kids. I felt comfortable during the process that he knew what to do during surgery to make it possible for me to have kids.
After surgery, we started preparing for IVF and I had my egg retrieval in July 2021. We ended up with 4 well graded, untested embryos after retrieval. My first FET (frozen embryo transfer) was in September 2021 and unfortunately ended in a chemical pregnancy. Shortly thereafter, we did another transfer and I gave birth to my son, Leo, on August 11.
Going through infertility takes a toll on you emotionally and physically. Here are a few pieces of advice I would give to other women dealing with infertility.
- Keep going even when it feels like you can’t do/go anymore. The little victories will give you strength. For example, the recovery from retrieval was brutal for me, but when we found out we got 4 embryos, I felt like I could do it all over again.
- Ask for help and allow help from others. I am the most organized person out there but I had to have my husband take the reins on the meds because it was all too much for me. I never prepared, mixed, set up, or gave myself one shot!
- Don’t change your lifestyle. Dr Miller never once told me what to eat, drink, do, or not do. Working out was limited with retrieval and FET, but that was the extent of it.
- Take the month off and go on vacation. Dr Miller wrote in my message on the portal that this was a must! You have to continue to live your life as best as possible!
COVID-19 Vaccine and Pregnancy/ Breastfeeding
Fertility History: Learning About Your Mom’s Fertility Journey to Help with Your Own
With a baby, who’s the first person you’ll usually call for help? If you’re lucky, your mom is usually only a phone call away to dispense parenting advice and tips for soothing a fussy baby.
But even before that, it’s a good idea to seek out her perspective on having children and the fertility journey she took to get there. When considering your own fertility history, you may want to consider digging into your family's medical past. The process of becoming pregnant can be a daunting task. And just as it helps to have a lot of support when the baby is born, you may want to have her help offer some insights into what you might face when it comes to pregnancy. Of course, you don’t have to tell her that you’re starting your own journey tomorrow or next week or even next month, but think of it as a perfect and valuable bonding opportunity between you and Mom.
You might be thinking, we aren’t the same person! How does her fertility history compare with yours? Well, for one, you can ask her about any medical conditions or fertility problems she faced when she was trying to get pregnant or during her pregnancy. It helps to gather some family history that the doctor may ask about, particularly if you may exhibit some similar traits. At the same time, while some conditions are genetically passed down, you should also be aware many other factors came into play during her pregnancies. Her age, health, environment, stress levels, diet, and your father’s health and lifestyle habits would all influence fertility and pregnancies. Not only that, modern medicine has changed so rapidly since you were born, so what might have been an issue for her back then may be handled or treated very different today.
However, talking to your mother, or even both your parents, can help give you more information than you realized you might need about your fertility history. Not only will you learn more about family medical history, but you’ll learn what it was like for them – the anticipation, the nervousness, the frustration, the questions they had for their doctor at the time. They may reveal some funny stories that you didn’t know before that might help you get excited about creating your own stories with your partner. You may realize that any fertility history questions or fears you had about family planning were not that different from what they went through to give birth to you.
Some fertility history questions you can start the conversation with:
- How long did it take for you to become pregnant?
- How old were you when you first decided to try?
- Did you have any issues?
- Did you have irregular menstrual cycles?
- Was there any family history of infertility?
- What about endometriosis, fibroids, or PCOS?
- Did you or any siblings ever have a miscarriage?
- Did you or anyone go into premature labor?
It’s also helpful to talk to any siblings, aunts, cousins, or even good friends about their individual journeys with pregnancy and their fertility history. Beyond the medical component, people often want to share their experiences, both good and challenging ones, and can help provide much needed support as you move through your own journey. Most importantly, you’ll realize that you’re not alone, and while everyone’s fertility story is their own, it’s a story that connects women on a profound and extremely special level.
Avoiding a Second Surgery: How a Change in Medication Could Lead to Pregnancy
Our last blog post detailed a successful isthmocele repair surgery that will hopefully lead to a healthy pregnancy. Today’s post is a little different.
Here is a case where surgery, performed by another surgeon, had failed. The patient, Lindsey*, was still symptomatic with fluid in the cavity. Dr. Miller provided the patient with a new medical protocol, avoiding a second surgery.
Read Lindsey’s story to find out the result.
After almost four years of struggling with secondary infertility, I was fortunate enough to discover Dr. Charles Miller and the Advanced IVF Institute. I had been diagnosed with an isthmocele, which was a defect in my cesarean scar that was leading to fluid accumulation in my endometrial cavity. Just reaching the diagnosis of an isthmocele and the potential impact it could have on my fertility had taken many years. I was exhausted, frustrated, and unsure if I would ever have another child. My local physicians seemed to be at an impasse. Despite having my isthmocele surgically repaired, I was continuing to develop fluid which was impairing the ability of my physicians to transfer any embryos.
After contacting Dr. Miller, I knew it was the right decision. He was very resolute in the forward management of my situation. He did not recommend a repeat surgery to repair the defect that had not been successfully repaired. This was initially surprising to me! Repeat surgery seemed to be the obvious decision, but his thoughts were that possibly changing the protocol for my Frozen Embryo Transfer (FET) would decrease the amount of fluid I was producing.
When transferring frozen embryos, the usual protocol is to use estrogen and the route can vary (i.e. oral, patch, intramuscular). The patient then adds progesterone prior to the transfer. Unfortunately, in my case, the estrogen caused a build-up of fluid, particularly with the isthmocele.
Due to his extensive experience in this matter, I trusted Dr. Miller’s judgment and I am so thankful that I did. After two previously canceled FET cycles with other protocols, I followed the protocol set forth by Dr. Miller on my third attempt.
The protocol that he recommended, and he said was successful on many occasions, is that rather than utilizing estrogen initially, the meds are used to stimulate the ovaries so that my own estrogen levels rise. Thus, taking away the need to utilize estrogen.
I am ecstatic to say that it worked and I am eternally grateful to Dr. Miller and his staff. We are set to welcome our miracle in May 2018!!
-Lindsey
*Name changed to protect patient privacy
Recognizing Gynecologic Cancer Awareness Month: The Importance of Hereditary Cancer Screening
Did you know September is Gynecologic Cancer Awareness Month? The five main gynecologic cancers consist of ovarian, uterine/endometrial, cervical, vaginal and vulvar. According to the Foundation for Women’s Cancer, more than 109,000 women will be diagnosed with a gynecologic cancer this year. That’s why it’s important to screen our patients regularly or recommend genetic testing if family history does in fact point to these gynecologic cancers.
Female gynecologic cancers can be sporadic, meaning, it doesn’t have to run in the family for the cancers to appear. You may not love your annual pap smear, but the quick, non-invasive test allows us to screen for cervical cancer and signs of pre-surgical changes. You also may dread the day of your screening mammogram, but it can help us detect changes to your breasts that cannot be felt with an exam, as well as early changes that are otherwise undetectable. If cancer is identified, our goal is to find it in its earliest stages to have better chances of eliminating it. As such, these screenings, although sometimes uncomfortable for you, can be lifesaving.
Despite the fact most cancers are not inherited, there are some family histories that are concerning for inherited forms of cancer. For example, when you visit your doctor, you are asked about your personal and family history for high blood pressure, stroke, diabetes and heart disease AND we also ask about any cancers in your parents, grandparents, aunts, uncles, siblings and children. If your family history does point to gynecologic cancers, we may recommend early and more frequent screening than the general population or determine you are a candidate for genetic testing.
Genetic testing evaluates your DNA (genetic material), and identifies whether you may have a genetic mutation (change in your DNA) that places you at an increased risk for developing different types of cancer, depending upon which mutation you have. Some mutations include the BRCA mutation that places women at increased risk for breast or ovarian cancer or Lynch syndrome that places one at increased risk for ovarian, uterine and colon cancer. It does not test your cells to see if you currently have cancer or will develop cancer, but instead gives you information on whether you have an increased risk of cancer compared to the general population.
Genetic testing involves counseling about what information the test can provide, the recommendations based on the test results, and the limitations of the test. If you and your physician decide that you are a candidate for testing, your blood is drawn and your results will return in 2-3 weeks. If you test negative it does not mean that you will never develop cancer, but rather you do not have a known inherited mutation that places you at increased risk for developing certain types of cancer. Conversely, if you test positive it also does not mean that you are definitely going to develop cancer, rather you have an elevated risk of developing certain types of cancer (range of 4%-80% risk depending upon the gene and type of cancer). For those that test positive, counseling can be provided and next steps will be discussed.
At the Advanced Gynecologic Surgery Institute, we are dedicated to you as your health advocate. We are here to offer you the best possible support and expertise through our many years of experience. If you want more information regarding hereditary cancer screening and testing, please contact our office: https://drcharlesmiller.com/request-a-consultation/.
To your continued health,
-Dr. Kirsten Sasaki
Her Own View: A Patient's Journey Through IVF (Days 4-11) Shots, Shots and More Shots
I have a few things to update. I started ovarian stimulation and had my first two monitoring appointments. The first appointment was 6 days ago and they took an ultrasound of the uterus to see what’s going on in there. They saw about 18 follicles on that first ultrasound, so they decided to start me on the Menopur (two vials), Follistim (150 units), Lovenox (one pre-filled injection) in addition to the Lupron. Yes, my friends, that’s four shots that I’m injecting into my belly every day! Some women want their husbands to do it, but I decided I wanted to do it myself. I think the mental aspect of taking four shots a day is a lot, and if you must coordinate with your husband to do these shots two times a day, it really adds another layer of complication--so, I stick myself! It’s kind of empowering, believe it or not!
Ok, the shots are NOT BAD! For the Menopur, I have to mix two vials of powder and one ML of solution. There are loads of tutorials on how to do this, so it’s not hard at all. This one does burn a little, but again, not too bad! Follistim is a pen, no mixing with this one. Burns a little, but again, it’s not bad. The Lovenox is by far the worst one. It burns going in. The first time I injected this one, it was PAINFUL! But, since that first injection, my expectations were set and I knew it was going to hurt. And now I’m used to it. If you make it this huge deal, then yes, it will be a huge deal. If you think of it as just part of your day, it’s no big deal. Wash your face, brush your teeth, give yourself your shot….done and done! Move on to the next thing! Also, I’ve not really felt any side effects. I’m bloated, but that could have just been the brownie I ate last night!

On the second ultrasound, they saw over 20 follicles, but all under 10mm. That means they are all small, and they need to keep stimulating me. After the appointment, they increased my Follistim to 300 units from the 150 I was originally on.
Dan and I also had to start an antibiotic to reduce the risk of infection at the time of retrieval. My next appointment is tomorrow, so I will update next week!
Thanks so much for reading!
-Katie
*Please note that each patient’s case is unique and Dr. Miller creates individual care plans for each couple based on their medical history.
Her Own View: A Patient's Journey Through IVF (Day 1-3)
Today we’re excited to share with you a new blog series about Katie, a patient of Dr. Miller’s, who has experienced difficulty conceiving. She will be sharing her fertility journey with us in her own words. Katie’s goal for journaling her journey, is that you might find comfort and strength in hearing from someone who is also going through the process as well, whether you are going through it now, or are pregnant after months (or years) of trying. Her struggle may be different, but her hopes and dreams of reaching the end goal, that bundle of joy, are the same. Although the outcome is unknown, Dr. Miller and his staff are excited to work together with Katie and her husband, Dan, as their partner and guide.
Hello Everyone!
My name is Katie and I would like to welcome you to my very first patient blog post! I’m excited to take this fertility journey with you. To give you some background, my husband, Dan and I are 31. After getting married in 2011, both Dan and I went to graduate school, which wasn’t the ideal time to start a family. Finally, at the end of 2015, we were ready to start our family. We officially started trying to conceive (TTC) in December 2015. To our surprise, we got pregnant the very first month of trying! Unfortunately, in March 2016, we lost the baby at twelve and a half weeks, a few short days after we told close family and friends. Since I had the miscarriage at home, we were not able to test for genetic abnormalities. My OB said over 50% of miscarriages happen because of genetic abnormalities, so that was most likely the reason. The entire experience was truly heartbreaking!
We were told by my OB to wait one cycle before TTC again. Since I had a D&C*, I didn’t get my first period until May 2016. In July 2016, we were pregnant again, which resulted in a chemical pregnancy* at 4.5 weeks. My OB decided to do a Recurrent Pregnancy Loss (RPL)* testing. Those tests indicated that I might have a blood clotting disorder; however, those tests were inconclusive.
My OB suggested we try again since my tests didn’t indicate any real red flags, but to take baby Aspirin for the possible blood clotting issue to be on the safe side. So we did try again, and we were pregnant again in October 2016, which resulted in another chemical pregnancy at 5 weeks. At that time, my OB agreed we should see a Reproductive Endocrinologist (RE).
After performing extensive online research, Dan and I decided to schedule a consultation with Dr. Miller in November 2016. I chose to see Dr. Miller because of his excellent reputation and success rates. Before he came in to see Dan and me, Dr. Miller reviewed my case. He said since I have an unknown reason for my recurrent losses, he would like everything tested-- from semen to genetics to blood. You name it, he’s testing it! Since I’m an HMOI patient, and Dr. Miller uses a lab outside the network, the tests had to be done through my OB.
The tests indicated that I have a MTHFR gene mutation*. This mutation does not allow synthetic folic acid to be absorbed into my body, so Dr. Miller gave me a prescription that would allow my body to absorb folic acid. I was hopeful that maybe this could be the answer.
During this time, Dr. Miller also had us do a Clomid* 50mg test cycle to see how my body would respond, but let us know that we would not be TTC just yet. We found that my progesterone was 15 Mg/Ml, lower than the 20 he likes to see with a medicated cycle. Perhaps this was another clue?
In early May 2017, we had our follow up appointment with Dr. Miller, and he talked us through all our options. He said the reasons for my recurrent losses are most likely due to a blood clotting issue or genetic abnormalities. He said we had three options:
- Clomid 100mg with Lovenox*
- IVF/ICSI* with Lovenox (50% live birth rate/ 16% chance of loss)
- IVF/ICSI with Lovenox and Preimplantation Genetic Screening (PGS)*. (70% live birth rate/ less than 5% chance of loss)
We decided to go for option 3! IVF with PGS!
So, here we are! We will do the egg retrieval in June and transfer in July! I’m currently on Lupron * 10 units, which I’ve been taking since May 23rd. Surprisingly, this injection is not bad at all. The needle is tiny and it’s relatively pain-free. I just got my period (finally!), making my cycle 32 days (very long for me as my average in 27 days). I’ll be starting my stimulation shortly here after an ultrasound in the coming days! The plan is to continue the Lupron and add Menopur* and Follistim*. The IVF nurses are really good at keeping me informed on next steps, and I also have a clear written protocol from the office.
I am cautiously excited about the next two months, but I’m not trying to get ahead of myself. I think the most important thing is to take it one step at a time, and not get too into my head about the whole process!
I’ll be updating on my IVF journey a frequently as I have new things to report!
-Katie
Katie's TCC Timeline
- 2011 – Married! Excited about life together!
- December 2015 – Removed the goalie! Let’s try to have a baby!
- March 2016 – 1st miscarriage at twelve and a half weeks. Heartbreaking. Maybe just an unfortunate fluke? Genetic abnormalities? Unknown. D&C to follow.
- July 2016 – Pregnant again! Chemical pregnancy 4.5 weeks. What’s going on here?
- August through September 2016 – Recurrent Pregnancy Loss (RPL) testing. Maybe a blood clotting issue?
- October 2016 – Pregnant again, and you guessed it…another loss at 5 weeks.
- November 2016 – Started seeing Dr. Miller. Discovered MTHFR gene mutation.
- March 2017 – Test Clomid cycle. Low progesterone.
- May 2017 – Starting IVF/ICSI with Lovenox and Preimplantation Genetic Screening (PGS). Taking Lupron 10 units since 5/23/17
- June 2017 – Got my period, waiting to go in for a baseline ultrasound and starting simulation for the retrieval!
Glossary
D&C: also known as dilation and curettage, a surgical procedure in which the cervix is opened (dilated) and a thin instrument is inserted into the uterus. This instrument is used to remove tissue from the inside of the uterus (curettage). ACOG
Chemical Pregnancy: occurs when the pregnancy hormone is elevated (i.e. beta hCG), but there are no other signs of pregnancy and it is too early to be detected via ultrasound (ivf.drcharlesmiller.com)
Recurrent Pregnancy Loss (RPL) Testing: examines genetics, infection, autoimmune testing, thrombophilia (blood clotting issues), the structure of the uterus and hormonal concerns (ivf.drcharlesmiller.com)
Clomid: Clomiphene stimulates the release of hormones needed to cause ovulation. Clomiphene therapy is typically used for 5 consecutive days early in the menstrual cycle, for 3 to 6 monthly cycles. It may take several cycles to find the right dose to stimulate ovulation. After that dose is determined, a woman will take the drug for at least 3 more cycles. If she does not become pregnant after 6 cycles, it is unlikely that further clomiphene treatment will be successful (ivf.drcharlesmiller.com)
Lovenox: Injections used to help prevent micro-clotting associated with Thrombophelia and or auto-immune deficiencies (ivf.drcharlesmiller.com)
IVF/ICSI: refers to a procedure designed to overcome infertility and produce a pregnancy as a direct result of the intervention. In general, the ovaries are stimulated by a combination of fertility medications and then one or more oocyte(s) are aspirated from ovarian follicles. These are fertilized in the laboratory (“in vitro”), after which, one or more embryo(s) are transferred into the uterine cavity. These steps occur over about a two-week interval of time, which is called an IVF cycle. (ivf.drcharlesmiller.com)
Preimplantation Genetic Screening (PGS): performed on cell(s) removed from a preimplantation embryo or a polar body from an oocyte. The goal is to identify de-novo aneuploidy in embryo(s) of couples presumed to be chromosomally normal. Theoretically, avoiding transfer of aneuploid embryos will reduce the risk of pregnancy failure and improve the probability of conceiving a viable pregnancy (ivf.drcharlesmiller.com)
Lupron: injection given below the skin, subcutaneous injection. These medications are used to enable the body to produce a higher number of quality eggs. These medications are also designed to prevent the mid-cycle hormonal surge which can result in a cancelled cycle. (ivf.drcharlesmiller.com)
Menopur: (menotropins for injection) is a prescription medicine that contains hormones. MENOPUR contains follicle stimulating hormone and luteinizing hormone activity. These hormones stimulate healthy ovaries to make eggs. (Ferring Pharmaceuticals)
Follistim: medicine that contains follicle-stimulating hormone (FSH) to help healthy ovaries to develop (mature) and release eggs; and as part of treatment programs that use special techniques (skills) to help women get pregnant by causing their ovaries to produce more mature eggs (Merck)
*Please note that each patient's case is unique and Dr. Miller creates individual care plans for each couple based on their medical history. Not all patients who have the MTHFR gene mutation will be treated with Lovenox.
Helping Women Navigate through Infertility and Reproductive Health Challenges
I’m excited to be writing the first post for our new blog! I say this all the time, but back in the day, when Michael Jordan and Oprah were in Chicago, I used to say I had the third best job in the city. With their absence, I guess I have the best! As a successful reproductive endocrinologist and minimally invasive gynecologic surgeon, I am fortunate enough to lecture around the world, conduct research and contribute scholarly articles to scientific journals and textbooks. However, what really motivates me is the opportunity to take care of you and help you achieve your health goals, and for many of you, help grow your family tree. That’s why this blog is for you.
I want this blog to be a resource for those seeking information about infertility treatment or gynecologic care. We will be discussing the latest in women’s health topics and sharing relevant information, research and news stories. I am so intrigued by all the medical and surgical advances we have seen since I was a medical student and look forward to sharing my thoughts as they continue to develop and expand. Not only will you hear insights from me, but also Dr. Cholkeri-Singh, Dr. Sasaki and other staff members.
I also hope to use this blog as a dialogue for my patients and anyone else who is looking for support with infertility or gynecologic care. I will write about topics you will hopefully find inspiring, offering you the strength and courage to continue to face treatments or surgery head on.
One of the best parts of being a physician is getting to know my patients and helping them resolve issues – whether it’s the resolution of pain and bleeding or finding just the right treatment plan to help a couple achieve pregnancy and fulfill their dreams of starting a family.
You’ll also hear from patients who will share their stories and journeys in hopes to show you that you are not alone in your struggle. It is a process – a very personal one, that can be long and with ups and downs -- and we are with you all the way through it.
My incredible staff will be highlighted in this blog. They are truly amazing and the backbone of my practice. Each month a staff member will be featured so you can get to know them better.
Lastly, I want to hear from you. Do you have questions about infertility, uterine fibroid treatment or endometriosis? Do you have a success story you would like to share that might give others hope? Drop us a line in the comments below or contact us through our website and be sure to follow our Facebook page.
To your health,
Dr. Miller







