PCOS Treatment Guidelines: Lifestyle, Medications and Fertility Options
This blog is the second part of Dr. Laurence Jacobs’ series on Polycystic Ovary Syndrome (PCOS). In part one, he discussed the signs, symptoms and diagnostic criteria for PCOS.
In this follow-up, Dr. Jacobs outlines the latest PCOS treatment guidelines, from lifestyle modifications and metabolic therapies to fertility medications and assisted reproductive technology (ART). PCOS is a complicated disease, understand your treatment options based on your fertility goals.
About PCOS
As discussed in part I, Polycystic ovary syndrome (PCOS) is characterized by a combination of excess hair growth, ovulatory dysfunction, and polycystic ovarian morphology on vaginal ultrasound, associated with insulin resistance. Latest treatment guidelines focus on lifestyle modifications, medications, and careful fertility care, including the role of newer agents such as GLP-1 receptor agonists.
Lifestyle Modification for Preconception Health
Lifestyle intervention, overlooked by many physicians for decades, remains the cornerstone of PCOS management. Weight management, improved nutrition, and physical activity are consistently associated with improved metabolic health, ovulation, and higher pregnancy rates. Even modest weight loss of 5–10% can often restore ovulation and/or improve pregnancy rates naturally, as well as with medication/IUI and IVF treatments. Programs that offer qualified medical nutrition therapy (MNT), regular exercise training, and behavioral modification via personalized provider telehealth have excellent outcomes for preconception health (WINFertility and OvumHealth).
Medical/Surgical Therapies for Weight and Metabolic Management
Metformin continues to be used as first-line pharmacologic therapy for metabolic abnormalities, such as impaired glucose tolerance and insulin resistance in women with PCOS. The supplement Myo-Inositol has also demonstrated significant benefit in dealing with insulin resistance.
GLP-1 receptor agonists (tirzepatide, semaglutide and related agents) are a major addition in the treatment options for weight loss. These medications significantly reduce body weight, and insulin resistance in PCOS patients. Current evidence also suggests improvements in menstrual cycle regularity and ovulation. They can be helpful as an adjunct to lifestyle changes for overweight/obese women but are most effective when used in conjunction with lifestyle improvements. Careful collaborative decision making is vital, as side effects (nausea, vomiting, pancreatitis, gallbladder disease, etc.), high costs with little insurance coverage and long-term safety remain an issue. Since pregnancy safety studies are lacking, contraception should always be utilized when GLP-1s are used in women planning pregnancy in the future and stopped when attempting conception.
Bariatric surgery may be considered for women with PCOS and severe obesity who meet criteria for surgical weight management. While not specific to PCOS, weight reduction from bariatric surgery may restore ovulation and improve metabolic health.
Laparoscopic ovarian drilling, another surgical option, has a very limited role in modern infertility practices, but in the past has helped some women by reducing ovarian testosterone and other male hormones (androgens). This option is rarely used today due to costs and potential damage to ovaries leading to adhesions.
Ovulation Induction and Infertility Management
Infertility is very common in PCOS, primarily due to anovulation and/or poor egg quality.
Letrozole has become the first-line medication therapy for ovulation induction in women with PCOS and anovulation, among most Reproductive Endocrine/Infertility specialists and many Ob/Gyns. Many well-controlled randomized studies have demonstrated higher ovulation, pregnancy, and live birth rates, as well as lower multiple birth rates with letrozole compared with clomiphene citrate.
Clomiphene citrate (Clomid) remains a popular option, particularly among Ob/Gyns. Combination therapy with clomiphene plus Metformin improves ovulation and live birth rates compared to clomiphene alone.
Metformin when used alone is less effective for ovulation induction but may be considered in combination with Letrozole and/or Gonadotropin medications (Menopur, Gonal F and Follistim), when doing ovarian stimulation for ovulation induction or IVF.
Gonadotropins are second-line therapy when oral ovulation induction fails. Careful monitoring is required to minimize the risk of ovarian hyperstimulation (OHSS) and multiple pregnancies. IVF is far more effective and safer regarding multiples.
Assisted Reproductive Technology (ART) and IVF
In vitro fertilization (IVF) is often reserved for women who fail less invasive ovulation induction therapies or who have additional infertility factors such as tubal disease or male factor infertility. In PCOS, IVF requires particular caution due to the high risk of OHSS. The newest guidelines emphasize the use of GnRH antagonist protocols (Ganirelix; Cetrotide) and individualized low dose stimulation strategies with Lupron triggers to minimize this OHSS risk. Pre-treatment with metformin may also reduce OHSS risk in women still undergoing IVF with GnRH agonist protocols. As noted above, Preconception care—including optimization of weight, hormones and metabolic status—is recommended prior to doing ART.
A Comprehensive Approach to PCOS Treatment
PCOS is a complex condition requiring an individualized, comprehensive approach. Preconception health with lifestyle modification remains first-line therapy. Medication therapy has improved. Metformin and Myo-Inositol supplements maintain their roles. GLP-1 receptor agonists, with proper counseling and informed consent, represent a new option for weight loss and metabolic improvement.
For infertility treatments, letrozole is clearly the first-line option for ovulation induction. Clomiphene, metformin (alone), and gonadotropins are occasionally used. IVF is very effective but requires careful strategies to minimize OHSS risk. Single frozen embryo transfers greatly reduce the risk of multiples. (1-2% identical, if embryo splits).
Expert Care for PCOS
Dr. Jacobs has helped women manage their PCOS for more than 40 years and was formerly the Director of the PCOS Center of Excellence. He understands firsthand how medications, supplements and lifestyle modifications can profoundly impact the health and fertility of PCOS patients.
If you think you may have PCOS or are struggling with symptoms, Dr. Jacobs and our team can help with the correct diagnosis and treatment options. Click here to schedule a consultation.
To understand more about PCOS, read part one of this blog discussing symptoms and diagnosis.
What to Expect at Your First Fertility Consultation with Dr. Jacobs
Starting your fertility journey can feel scary and intimidating, yet also hopeful. Knowing what to expect can help ease anxiety and make you feel more comfortable before beginning this process.
With more than 45 years of experience, Dr. Laurence Jacobs has guided thousands of families through their fertility consultations. Here’s what to expect when you schedule yours:
First Steps:
You and your partner (if applicable) should plan to attend the first consultation together; it usually lasts about an hour.
What We’ll Review:
- Medical records and history, menstrual cycle, past surgeries or complications
- Lifestyle factors and any medical issues (for you or your partner)
After that, we’ll outline the infertility workup to determine why pregnancy isn’t happening. This includes:
- Hormone blood tests
- Diagnostic ultrasounds
- X-rays
- Semen analysis
5 Key Fertility Factors We Evaluate (you may have more than one)
1. Male Factor
- Semen analysis
- Sperm function test, including strict morphology, to identify if there is any difficulty in being able to fertilize an egg
2️. Ovarian Reserve (Egg Supply)
- On cycle days 2-4, you will come into the office so we can check your hormone levels, including AMH, which helps assess your egg supply.
- We’ll also do an antral follicle count transvaginal ultrasound to measure how many egg sacs (follicles) are present. The sonographer will count the antral follicles on both ovaries, looking for them to be 2-10 mm in diameter. The more follicles the better!
3️. Ovulation Evaluation
- Ovulation predictor kits, which look for a rise in a hormone called LH that tells us when you’re about to ovulate
- Ultrasound to check egg sac (follicle) size
- Follow-up progesterone test about a week later to confirm ovulation and assess if you have produced enough progesterone to be able to build up the lining of the uterus to get it ready for a pregnancy
4️. Uterine and Tubal Factors
- HSG, an X-ray using contrast dye, to view the uterus and fallopian tubes or a saline sonogram to check for fibroids, adhesions or polyps
- We also flush the fallopian tubes (part of the HSG) to make sure the fluid goes through the tubes so we know if the tubes look healthy and are functioning properly.
5. Pelvic Factors
- Check for adhesions from endometriosis, pelvic inflammatory disease or past surgeries
- Assessment for fibroids that could impact fertility
Next Steps:
After your workup (typically completed in a few weeks), we’ll schedule a follow-up appointment to review results, discuss medications and consider options like IUI or IVF if necessary. We’ll also recommend lifestyle changes to help support your fertility.
Ready to schedule?
Call us at 630-428-2229 or fill out this request form to get started.
About Dr. Laurence Jacobs
Dr. Laurence Jacobs is a Mayo Clinic fellowship-trained Reproductive Endocrinologist with over 45 years of experience helping thousands of families build their dreams through personalized fertility care.
Board-certified in Obstetrics and Gynecology, Dr. Jacobs brings deep expertise in IVF, PCOS, male and female infertility and second opinions for complex cases. After decades in leadership and practice, he is proud to provide consultations at Charles E. Miller, MD & Associates | CCRM Fertility’s Naperville office. Known for his compassionate approach and trusted by both patients and peers, Dr. Jacobs has been recognized nationally as a Top Infertility Doctor and consistently honored for his patient-centered care.
Patient Story- Kayla
For many couples, the dream of starting a family is filled with excitement and anticipation. But for Kayla and her husband, that dream turned into a struggle with infertility. Just when they thought they had reached the end of the road, a second opinion with Dr. Miller changed everything. This is their story and the journey to two little boys that made it all worth it.
Like most couples, we dreamt of starting a family filled with laughter, love and the pitter-patter of little feet. However, as months turned into years, that dream seemed to drift further and further from our grasp. What began as hopeful anticipation soon gave way to the harsh reality of infertility. Month after month, we watched as the lines on pregnancy tests remained stubbornly blank, each negative result a painful reminder of our unfulfilled longing. Faced with the heartbreaking prospect of infertility, we embarked on the difficult journey of fertility treatments.
With our hearts full of hope, we began our fertility journey. We spent a year at our initial fertility clinic before finding Dr. Miller. Within that first year, we underwent numerous tests yielding frustratingly normal results and a series of treatments that encompassed Clomid, IUI and eventually IVF. Our first IVF round yielded 11 embryos. With eager anticipation, we underwent a fresh transfer and subsequent frozen transfers, clinging to the belief that each embryo held the key to our future family. However, amidst our prayers and unwavering determination, we encountered the bitter sting of disappointment in the form of only one chemical pregnancy.
Despite our best efforts, the road to parenthood seemed full of overwhelming obstacles. Faced with the crushing blow of yet another failed attempt, our doctor delivered the devastating news that there was nothing more he could do for us. With our hearts shattered, we made the decision to seek a second opinion.
When we first met Dr. Miller, we felt defeated and hopeless. However, we were determined to leave no stone unturned before exploring other alternatives. Seeking a second opinion turned out to be a pivotal moment in our journey to parenthood, leading us to the greatest gifts of our lives. Through three rounds of IVF under Dr. Miller’s guidance, we experienced a rollercoaster of emotions, each cycle marked by its own unique challenges and triumphs.
In our first round, despite our renewed hope, we faced yet another heart-wrenching setback with another chemical pregnancy.
After years of tirelessly chasing the elusive dream of parenthood, we found ourselves on the brink of surrender. We had spent years going through countless treatments and tests to only find ourselves right back where we started on our journey to parenthood. Despite the pain and disappointment, we made the courageous decision to give it one last chance.
Our second round of IVF with Dr. Miller was a life changing moment in our journey, etched in our hearts as a turning point that brought light to the darkest days. We were initially filled with hope as 12 embryos seemed to be thriving. However, the day of our fresh transfer, our hopes were crushed when we learned that only one embryo had survived. Little did we know, that single embryo would become our greatest blessing, our precious son Theodore.
We became pregnant in January 2020, just before the world was engulfed by the chaos of the Covid-19 pandemic. We felt extraordinarily blessed. In a time of uncertainty and fear, our joy was immeasurable as we welcomed the news of our pregnancy. It was a reminder that amidst the darkness, miracles still happen, filling our hearts with hope and gratitude for the precious gift of new life.
After experiencing the immense joy of welcoming our first son into the world, we knew in our hearts that we wanted to expand our family and give him a sibling. Returning to Dr. Miller, we embarked on another round of IVF. Starting from scratch without any frozen embryos. This time, our efforts blessed us with eight precious embryos, one of which would become our beloved son, Cameron.

Our journey to parenthood was marked by highs and lows, hope and heartbreak, yet it led us to the most precious gift of all- our two sons. Their arrivals into our lives was nothing short of miraculous. Despite the challenges we faced along the way, we are forever grateful for modern medicine and our doctors, nurses and countless others who played a role in making our dreams a reality. They have given us the greatest gifts of all time, and for that, we will be eternally grateful.
-Kayla
Patient Story- Chloe- Asherman's Syndrome

Today we are featuring Chloe’s patient journey with intrauterine adhesions. According to Dr. Miller, these adhesions are one of the hardest things to deal with in infertility. Chloe sought Dr. Miller’s help after a pregnancy loss and being diagnosed with Asherman’s syndrome, a condition where adhesions form inside the uterus. Dr. Miller performed surgery to remove the adhesions and Chloe participated in a clinical trial aimed to prevent the return of these adhesions. The surgery was successful and Chloe recently welcomed her daughter, Charlotte. We are so happy to have played a part in helping Chloe become a mother.
Check out Chloe’s story:
In September 2021 we found out that we were pregnant with our first baby and we were over the moon. Fast forward to January 2022 and we lost our little boy when I was 23 weeks pregnant. We were distraught and didn’t know what to do. On top of losing our baby I was then diagnosed with Asherman's Syndrome. According to the Cleveland Clinic, Asherman’s syndrome is an acquired condition where scar tissue (adhesions) form inside your uterus. The scar tissue can build up, decreasing the amount of open space inside your uterus. Women with Asherman’s syndrome may experience light or no periods, pelvic pain or infertility.
We weren’t very educated on this syndrome at the time, but later on found out that it would be difficult to get pregnant with Asherman's syndrome. I was told that I would need a hysteroscopy to get rid of these adhesions. A hysteroscopy is a procedure in which a surgeon inserts a thin, lighted telescope to see inside the uterus. Adhesions can be removed at this time.
I knew that I wanted to make sure I had the best doctor performing this procedure since my ability to have kids depended on it. I learned about Dr. Miller from my husband's cousin, who is a nurse in Park Ridge. At the end of 2022 I scheduled an appointment. Dr. Miller ended up performing the hysteroscopy and lysis of adhesions in March 2023. I took part in a clinical trial to get rid of my adhesions. The trial looked at the effect of a soft gel-like material, called Juveena™ Hydrogel, inserted into the uterus after the removal of adhesions to reduce the formation of adhesions again.
After my procedure the nurse told me that my adhesions were some of the worst she had ever seen. However, they felt like they had gotten all of them. I had a follow up a few months later where I was told everything looked good and I was ready to try for another baby.
In November 2023 I found out that I was pregnant again. My husband and I were very excited, but also nervous after everything we had previously gone through. Dr. Miller and his team were great from the moment I told them that I was pregnant. They got me in for a visit right away and started monitoring me until they felt I was in the safe zone.
In June we welcomed a sweet little girl named Charlotte into the world. We are so in love with our baby and so thankful to Dr. Miller and his team. If it wasn’t for him I truly don’t believe we would have Charlotte. I know if I have any issues in the future Dr. Miller would be the first person I would reach out to.
Do's and Don'ts During the Two-Week Wait After Embryo Transfer
Transfer Day is an exciting and hopeful point on your fertility journey, but the two-week wait that follows can be a challenging period filled with stress, anxiety and impatience. To help you make the most of this crucial time, we consulted with Monika and Mel from our amazing IVF team. They shared some important do's and don'ts to help you through the two-week wait post embryo transfer.
❌Don't Google - Trust Your Medical Team for Guidance
We know it’s tempting, but one of the most common instincts during the two-week wait is to turn to Google for answers and reassurance. However, this can lead to unnecessary stress and confusion. Remember your fertility journey is unique to you and best understood by your medical team. Rely on their expertise and guidance to ease your concerns and not Dr. Google.
✅Follow Medication Instructions
Unless instructed otherwise by your doctor, make sure to continue your medication regimen. Medications like progesterone help support embryo implantation. Consistency in following your doctor's orders is key to your success.
❌Don't Take a Pregnancy Test
It's natural to be anxious and eager to confirm a positive outcome, but taking a home pregnancy test too early can be inaccurate and potentially lead to disappointment. These tests may show a negative result because it's too soon to detect the necessary hormone levels. Or, in some cases, they might show a positive result, but the pregnancy may not continue to develop as expected. Instead, wait for the blood test, which provides more accurate and reliable results.
✅ Rest on Transfer Day, but Stay Active
While it's important to take it easy on the day of the embryo transfer, this doesn't mean you need to spend the entire two weeks in bed. Light activities such as walking can actually help boost blood flow, potentially benefiting the implantation process.
❌ Don’t Have Sexual Intercourse
To support the best conditions for the embryos to implant, refrain from sexual intercourse and orgasm during the two-week wait. This helps prevent uterine contractions that may interfere with the process.
✅ Do Delay Having a Bowel Movement
After the embryo transfer, it's wise to avoid any activities that might strain the pelvic area, including pushing during a bowel movement. Wait for about 5 hours before trying to have a bowel movement.
❌ Don't Drink Alcohol
During this critical period, it's best to maintain a healthy lifestyle, including your diet. Avoiding alcohol and focusing on a well-balanced diet is essential.
✅ Try to Relax and Manage Stress and Anxiety
Stress and anxiety are natural during the two-week wait, but managing these emotions is crucial. Consider relaxation techniques such as acupuncture, yoga, journaling or simply pampering yourself. A calm mind supports your fertility journey.
Always remember to follow the specific instructions provided by your dedicated care team. They are here to support and guide you through this journey. You're not alone, and we're here for you every step of the way.
For any concerns or questions, don't hesitate to reach out to our team. We're here to provide the care and assistance you need.
Patient Story- Breda
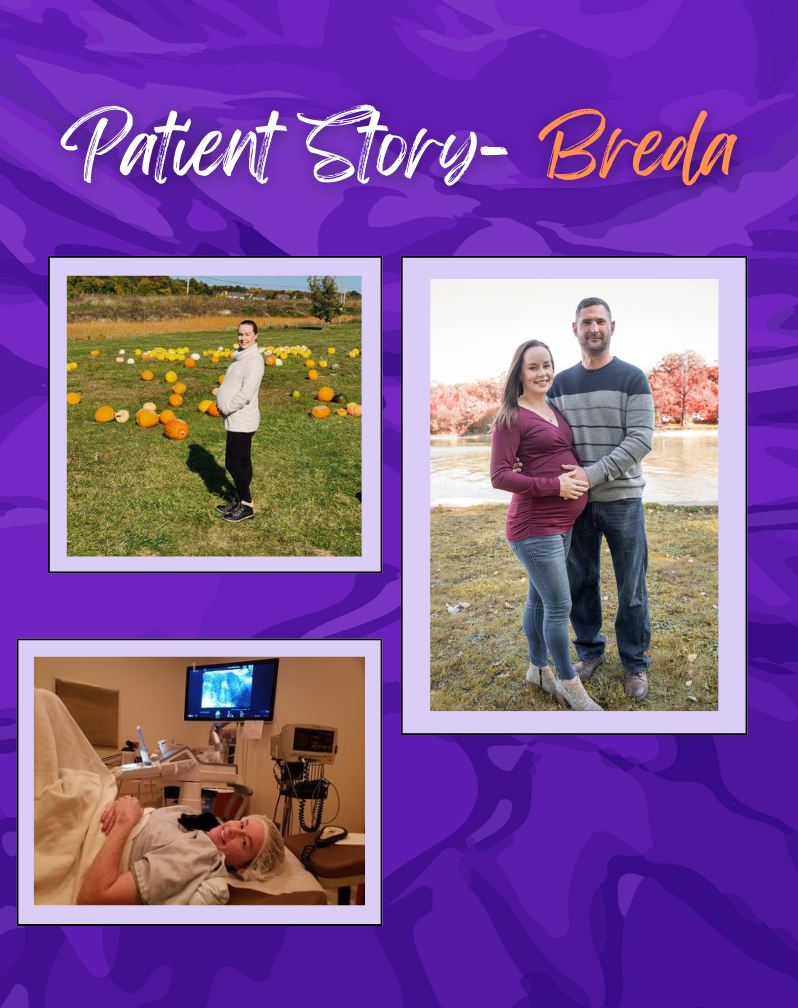
“Not everyone will understand IVF or be able to relate, so it’s important to surround yourself with support. More people than you realize struggle with infertility.”
Today’s patient story is from Breda. After not finding success or feeling comfortable at another fertility clinic, Breda came to us. We are all glad she did! Dr. Miller was able to diagnose her with endometriosis and after surgery and IVF, she was able to get pregnant. Breda is due in January!
Breda writes:
I met my husband later in life and we got married when I was 38. I was and still am wary of the stigma of older mothers, even though being older is accepted. I’ve always wanted a family and we started trying right away, but I had three miscarriages in a year and a half. I was at a different fertility clinic for a year, but didn’t feel comfortable there. My husband’s colleague recommended we see Dr. Miller and what a difference!
We first met online during COVID and Dr. Miller told us, “You’ll be a mother, kiddo.” He was so kind, didn’t rush us, and he explained everything. He learned I was an English teacher and told me a story that put me at ease. He never stopped his storytelling, and I welcomed his personable demeanor after some bad experiences at the previous clinic. Dr. Miller found issues that the previous doctor did not, including endometriosis.
After a biopsy, Dr. Miller found abnormalities in my uterus and I was diagnosed with Level 1 endometriosis. During surgery, he removed five spots on my uterus. I also had the Endometrial Receptivity Assay biopsy to determine the receptivity of the uterus to implantation. Soon after, we had an egg retrieval and two transfers.
Throughout this process, Dr. Miller and his staff explained everything so thoroughly and never seemed irritated or disinterested when I had questions. I also got to know Dr. Miller and the nurses because they talked to me during appointments. I always felt people cared and were invested in our success. I felt so secure going into our procedures and never felt anxiety or stress visiting the office.
Even though our first transfer failed, a second embryo implanted and I will never forget that experience. Dr. Miller, Courtney, and Melody were present for the transfer, and made me feel so comfortable. Dr. Miller even told us a funny story about meeting an actor from Will & Grace. While we waited after the transfer, my husband and I held hands and prayed, and we also talked about how wonderful it would be if it worked. Many times, we dreamed of finishing our nursery and being able to move forward with our plan. The transfer worked, and our baby is due January 8, 3.5 years after we began IVF and what seems like a million doctor appointments.
I was very nervous the first 12 weeks of my pregnancy and braced myself for bad news, but at every ultrasound Courtney reassured me with her positivity. We are so grateful for everyone at the Naperville office.
It took until I was about 20 weeks pregnant for me to relax and realize we’re finally going to be parents! I’ve cried many happy tears for a change! Not everyone will understand IVF or be able to relate, so it’s important to surround yourself with support. More people than you realize struggle with infertility. Meditation and journaling are helpful (as well as long walks with our dog, my first baby). Finally, never stop hoping and praying, even if you’re an older mother!
Patient Story- Molly
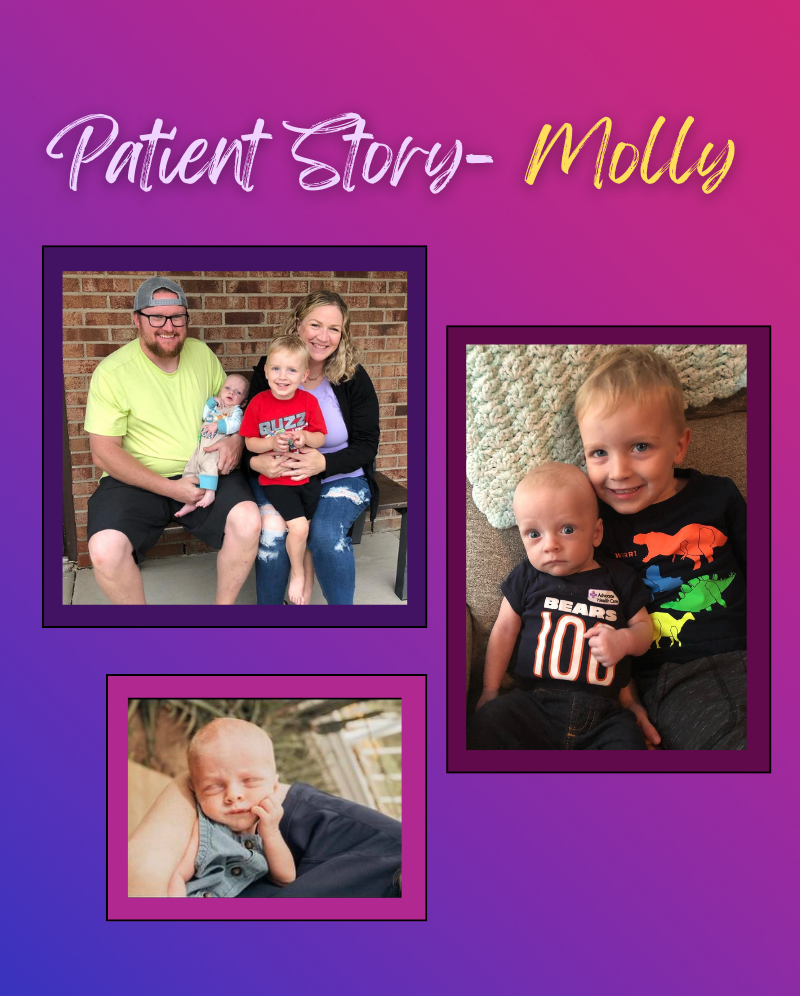
“We have been so blessed that I know all the pain and suffering we endured was worth it.”
We’re featuring Molly’s story today! Molly’s story is unique because she was diagnosed with unexplained infertility. This is a tricky diagnosis, because even after testing a cause cannot be determined. When this is the case, there is a lot of trial and error in order to achieve pregnancy. But as Dr. Miller always says: “Trust the process.” That’s just what Molly did and now she has two beautiful sons. Read her story below.
I first became a patient of Dr. Miller’s in 2012 when I had a myomectomy, a surgical procedure to remove uterine fibroids. After getting married and trying for several months to get pregnant, a co-worker suggested I see Dr. Miller, but this time as a fertility specialist. At our first appointment, Dr. Miller ordered blood work and a hysterosonogram which is an ultrasound exam that provides images of the inside of the uterus to help diagnose the cause of abnormal vaginal bleeding. However, everything came back fine. I was told I had unexplained fertility. This wasn’t the news I wanted to hear! It would have been easier to have a specific reason for why I could not get pregnant.
I was put on medication for thyroid and prolactin issues. After a month on the medication, it was advised we try an IUI. We failed all three attempts. Dr. Miller said IVF would need to be our next step. Soon after, my retrieval resulted in 26 eggs! My husband and I were so excited, our dream of having a baby was one step closer.
However, we were unable to do a fresh transfer at that time because I was borderline for Ovarian Hyperstimulation Syndrome (OHSS). This occurs when a woman’s ovaries swell and leak fluid into the body. This condition is temporary and occurs in less than 5% of women who receive fertility treatments. Instead, we ended up freezing 8 embryos. About two months later one embryo was successfully transferred. It was a strange feeling, because I was so happy and terrified at the same time.
After graduating from Dr. Miller’s office, my OB/GYN monitored me closely and that little embryo was born at 34 weeks gestation. Again, I was happy and terrified at the same time. Thankfully our little boy was healthy and strong.
After our son turned 18 months, we decided to start the process to have another child. We decided to follow the same protocol as before and do a transfer in three months. Unfortunately, it failed. After meeting with Dr. Miller again, he advised us to do a trial cycle with an Endometrial Biopsy (EMB). An EMB tests whether the uterine lining is preparing itself adequately for implantation of the embryo. If the lining is out of phase, it can prevent implantation from occurring or result in an early miscarriage. Because the results of my EMB were abnormal, I was treated with progesterone. The following month we had another transfer and it was successful! We welcomed our second baby boy this June./p>
Our two little boys are thriving! We are so happy we found Dr. Miller and are so grateful for everyone in the office as well as Dr. Deutch who did our last transfer. Our advice to other couples going through infertility is to know that you are strong, brave and deserve to be parents. Don’t ever give up! We have been so blessed that I know all the pain and suffering we endured was worth it.
COVID-19 Update (April 2, 2020)
COVID-19 and Fertility: Update
[PLEASE SEE OUR APRIL 2 UPDATE ON THIS]
These are the most recent recommendations from the American Society of Reproductive Medicine (ASRM). I have spoken with a number of reproductive endocrinologists in the area as well as Lisa Ray, our embryology director. I do realize that there are 9 cases in China where women diagnosed with coronavirus did have successful pregnancies. Unfortunately, the numbers are too small to ultimately know the risk to mother and baby with this novel coronavirus.
Therefore, based on ASRM’s recommendations, the discussion with my peers and my own concerns with potential risks in pregnancy (i.e. heightened risk to the mother of coronavirus due to pregnancy and the potential problems with diagnostic studies and treatment, if a pregnant woman has severe complications due to Coronavirus), at present, our team is proceeding as follows:
- Patients on Clomiphene Citrate and gonadotropins should stop their cycle and not attempt pregnancy either via inseminations or timed intercourse. However, if the couple is inclined to proceed with cycle completion (inseminations and timed intercourse), they must sign a waiver stating that they understand the unknown risk to mother and baby in regards to the virus. Otherwise, the cycle will be cancelled. No new cycles with Clomiphene Citrate and gonadotropins will be initiated.
- Women who are currently undergoing IVF stimulation can proceed with their cycle. We do recommend a freeze‐all with the caveat that fresh transfer can be considered if it is deemed that freezing of the embryos/eggs would be detrimental to successful pregnancy. Once again, a waiver must be signed stating that at present, the risk of subsequent transfer of coronavirus-infected embryos/eggs, although believed very low, is ultimately unknown to mother and baby. Furthermore, it must be understood that these cycles may be stopped at any time given further recommendations from the ASRM.
- Because of the anticipated increase in the coronavirus, the ASRM has recommended that no new stimulations be started. However, as this is solely a recommendation, for the immediate future, we will continue to evaluate stimulation starts on an individual basis; again, with the recommendations as outlined above (i.e. freeze‐all of embryos/eggs, waiver must be signed, cycles may be stopped, etc.). Please contact our office regarding your individual cycle concerns.
- In regards to patients who already have frozen embryos and wish to proceed to frozen embryo transfer and are currently on medication, once again, the risk of pregnancy in a patient who is positive for Coronavirus is unknown. Therefore, our recommendation is to not proceed at present. However, if a couple wishes to proceed, they need to be aware that we will support them in their decision, but will require them to sign a waiver. This decision could change at any time.
Thank you,
Charles E. Miller, MD FACOG
ASRM Issues New Guidance on Fertility Care During COVID-19 Pandemic: Calls for Suspension of Most Treatments
3/18/2020 The American Society for Reproductive Medicine (ASRM), the global leader in reproductive medicine, today issues new guidance for its members as they manage patients in the midst of the COVID-19 pandemic. Developed by an expert Task Force, of physicians, embryologists, and mental health professionals, the new document recommends suspension of new, non-urgent treatments.
Specifically, the recommendations include:
- Suspension of initiation of new treatment cycles, including ovulation induction, intrauterine inseminations (IUIs), in vitro fertilization (IVF) including retrievals and frozen embryo transfers, as well as non-urgent gamete cryopreservation.
- Strongly consider cancellation of all embryo transfers, whether fresh or frozen.
- Continue to care for patients who are currently ‘in-cycle’ or who require urgent stimulation and cryopreservation.
- Suspend elective surgeries and non-urgent diagnostic procedures.
- Minimize in-person interactions and increase utilization of telehealth.
The above recommendations will be revisited periodically as the pandemic evolves, but no later than March 30, 2020, with the aim of resuming usual patient care as soon and as safely as possible. ASRM has been closely monitoring developments around COVID-19 since its emergence. Data on its impact on pregnancy and reproduction remains limited. However, the task force used best available data, and the expertise and experience of the members to develop the recommendations. Until more is known about the virus, and while we remain in the midst of a public health emergency, it is best to avoid initiation of new treatment cycles for infertility patients. Similarly, non-medically urgent gamete preservation treatments, such as egg freezing, should be suspended for the time being as well. Clinics who have patients under treatment mid-cycle should ensure they have adequate staff to complete the patient’s treatment and should strongly encourage postponing, the embryo transfer.
Catherine Racowsky, President of ASRM, noted, “ASRM is striving, as we always do, to ensure our members have the very best information available as they care for their patients. We are all facing a great deal of uncertainty, but we do know our health care system is about to be stressed in a way it has never been stressed before. Only by working together medical professionals, patients, citizens of an inter-connected world, can we hope to meet this latest challenge.”
Ricardo Azziz, CEO of the ASRM stated, “This is not going to be easy for infertility patients and reproductive care practices. We know the sacrifices patients have to make under the best of circumstances, and we are loath to in add, in any way. to that burden. And it will not be easy for our members. The disruption to routines, the stress on staff members and the very real prospect of economic hardship loom large for ASRM members all over the world. But the fact is that given what we know, as well as what we don’t, suspending non-urgent fertility care is really the most prudent course of action at this time.”
Dr. Racowsky added, “We should recognize that the situation on the ground is fluid, and as such we will continue to revisit and review our recommendations at least every two weeks, to provide providers and their patients with the best information and support we possibly can.”
For almost a century, the American Society for Reproductive Medicine (ASRM) has been the global leader in multidisciplinary reproductive medicine research, ethical practice, and education. ASRM impacts reproductive care and science worldwide by creating funding opportunities for advancing reproduction research and discovery, by providing evidence-based education and public health information, and by advocating for reproductive health care professionals and the patients they serve. With members in more than 100 countries, the Society is headquartered in Washington, DC, with additional operations in Birmingham, AL. www.asrm.org
A Note About COVID-19 From Dr. Miller
Please see our 3/18/20 update about COVID-19 and fertility treatments.
Dear All,

