Infertility Doesn't Discriminate
Families are made up of many different sizes and types. There are parents and children, grandchildren, grandparents, sometimes great-grandparents, aunts, uncles, cousins, far-removed cousins, even pets. In my grandchildren’s case, there are stuffed lovies. Don’t even try to suggest to them that they are not part of the family.
I get similar types of families through our doors. Naturally, all of them are people who wish to become parents one day or to grow their existing families. They come from all walks of life and backgrounds. Some are heterosexual couples. Some are same-sex couples. Some are married, others not. Some are single or widowed. Some are disabled. Some are cancer patients, hoping to plan for a future family. Some are financially well-off, others are less so.
Despite the wide range of people who come visit our offices, the overarching sentiment is the same: Love. Love for their partner and for the future child they hope to have. Love for their own parents, who they want to make into grandparents.
Of course, there is another unifying theme: struggle.
Infertility is hard. It’s a difficult realization to grasp, and the journey of fertilization can be emotionally taxing, not to mention physically. It’s a huge waiting game, one that requires a lot of patience. We try hard not to add to the struggle but just to be the scientific voice in the whole messy equation. All of our patients persevere bravely through the process.
Infertility selects at random. It doesn’t matter what your background is or where you are in your life. It doesn’t discriminate, and neither should anyone else.
Lastly, there’s one unifying trait. Desire. To be a parent. To be able to one day hold a baby in their arms, care for it, raise it, watch it grow up. The people who walk through our doors have thought this thoroughly, done the research, made the decision to go forward with the process. And it doesn’t matter what their background is – they are prepared, they are knowledgeable, and they are willing to do whatever it takes to dedicate their lives to a little human being.
These people will be good parents.
For all these reasons, I know that every one of my patients deserves to be a parent and to have that chance to give themselves fully to another human being. We support every one of our patients’ decisions to give fertility a chance, and we believe that no one, even their own bodies, should tell them otherwise.
Keeping Hope Alive: My Infertility Journey
In 2009, I married my best friend. Joe was loving, fun, a protector and my perfect match. He loved going out, being social and living in the moment. He was okay to never commit or have children. But that all changed when he met me.
One warm April day I got in a car accident. Joe was the responding officer, and he wrote me a ticket! But Officer Joe saw me in distress and panic, and offered to drive me home. Talking about where I was headed, we quickly learned that we had mutual friends at the restaurant where I worked. Let's just say these friends made this relationship happen.
Over the next few months of dating, I learned Joe had testicular cancer years ago and was already in advanced stages when he found out. He quickly had surgery and started chemotherapy a few weeks later. His family encouraged him to bank his sperm, but his doctor assured him the type of chemo he was using would not affect his fertility. Since Joe always planned to be single and never have children, there was no need to bank. But when he met me in 2005, I told him on our first date that it was my dream to have children. Needless to say, he changed his mind and wanted a child just as much as me.
Fast forward to September 2009: beautiful wedding, perfect life. We decided to start trying for a child in 2010. First month, nothing. Next month, nothing. 12 months later, nothing. We decided to get help. I scheduled an appointment with my ob/gyn and had tests conducted in November 2011 that determined I was not ovulating on time. He also wanted me to have a scan.
Concurrently, Joe's doctor wanted him to complete a sperm analysis. The office called and left a message saying that "everything looked good." During my scan, they determined I had what is called a septate uterus. Which means my uterus had tissue that divided it and that makes it difficult for an embryo to implant. My ob/gyn wanted to schedule surgery to cut the excess tissue out. Joe and I decided we needed a second opinion so we called a fertility specialist.
When we were meeting with the doctor, he turned to Joe and asked for the results of his sperm analysis. Five minutes later, a nurse retrieved our results and our world was rocked. Joe's analysis stated he had ZERO sperm. He wasn't okay. Our minds were blown to say the least. Then he asked us if we were open to adoption because we could never have children. We stood up crying in disbelief and left the office.
After doing some research and talking with my cousin who was an ob/gyn doing her fellowship in fertility, she recommended we visit a urologist and see if there was a way to "go in and get them". After seeing three different urologists over the course of four months, Joe had to start taking injections to prep for the TESE surgery in which sperm is surgically removed. Wouldn't you know in this six month span, our fertility specialist retired? Now we had to find a new one.
We were referred to Dr. Miller at the Advanced IVF Institute by many friends. They talked about everyone from the receptionists, nurses, and doctors. "They work miracles there," they said. Our first appointment with Dr. Miller was in late March of 2012. He looked over our file and said, "We are going to get you pregnant." He prepped us on the schedule of everything, including surgery to remove the septum and coordinating with the Urologist to prep Joe for surgery. Joe and I left the office that day smiling over our infertility struggle for the first time in two years.
In July of 2012, I had my surgery to remove the septum from my uterus. Everything went as planned and we were ready to proceed with ICSI, a type of in-vitro fertilization where a single sperm is injected into an egg. Over the next few months we had countless appointments with both Dr. Miller and the Urologist out of Northwestern. We had to wait for Joe to be at a certain level of testosterone in order to do surgery.
Fast forward a few months, and the doctor stated we were at the highest level he would ever be. It was time to start prepping me for my egg retrieval AND choose an anonymous donor sperm just in case Joe's surgery wasn't successful. Because we knew the TESE surgery was only a 50/50 shot, we had to have donor vials waiting after the retrieval. This was a huge obstacle as Joe was not sure how he felt about using donor sperm.
Over the next few weeks, I mulled through the cryobank checking for common traits and examining the donors’ health records. Finally, I found the perfect one! In April of 2013, my eggs were retrieved in Dr. Miller's office, while Joe was in the next room having TESE surgery.
After we both woke up, Dr. Miller informed us my retrieval was very successful and they retrieved 19 eggs. However, the Urologist did not have any good news. Joe had ZERO sperm, and they believed he may have been born infertile, so the donor sperm was used. Our worlds were rocked again! Days after the surgery, I ended up hyperstimulating and they had to cancel my transfer because of the swelling. However, the good news was we had 14 embryos fertilized. We were informed about the freezing process and discussed that many embryos would not mature normally to the freezing process at five days. We did and ended up with six viable embryos.
The following month, once again I was prepped for a transfer through hormones and many doctors’ appointment. Five days before my transfer I went in for the final check to start the progesterone shots. What the doctor and nurses told me was startling. My uterus was full of fluid and they had to once again cancel my transfer. Two weeks later, I went back to Dr. Miller and he did a quick procedure to ensure the septum wasn't growing back. It appeared that it was, so he once again scraped it out.
Unfortunately, this prolonged the next transfer. We had to wait until October to transfer our frozen embryos. We waited anxiously for the date, and began prep. Our transfer finally occurred on November 2, 2014. Two embryos survived the thaw and were implanted. I was over the moon!
Ten days later, I returned to the office for my pregnancy blood draw. I went to work that day like it was any other day. I knew my nurse usually called me around 1:30 pm with my results from the mornings' tests. At 1:32, my phone rang. It was my nurse and she didn't sound positive... She told me that I wasn't pregnant... I quickly gathered my belongings and called my principal to get me a substitute. Then I ran out of my building and got in my car sobbing and shaking. I called my husband and he assured me it was going to be okay. This just wasn't our time, but that time would come.
The next day, I returned to the clinic for more testing. Again, not pregnant. Joe and I met with Dr. Miller a week later to discuss the failed cycle. Without genetic testing, the most likely reason for implantation failure is a genetically abnormal embryo. We decided that we would try again. Before we did though, he wanted to check my uterus for scar tissue from the surgery. 4 weeks later and another quick procedure, we got the clearance to begin our next cycle. On February 16, 2015, Joe and I entered Dr. Miller's office. We laughed and talked to our nurses and they comforted us in the situation. And then they transferred 2 more embryos while I was put under.
The next ten days waiting to do my pregnancy bloodwork were the longest days of my life. Joe and I were building a house at the time, so we tried to keep ourselves busy. Then on February 26th, I entered the office for my bloodwork. I continued to work as always, but I asked my nurses not to call me until after school. Every five minutes though, I kept checking my phone. The dismissal bell rings at 3:15pm At 3:14, I saw my phone light up... the bell hadn't rung and my students were cleaning up and organizing to leave for the day, but I couldn't miss this call.
I picked up the phone and I heard Patty's voice. "Danielle." I quickly asked her to hold on... the bell rang, I said goodbye to my students and picked up the phone. "Danielle... you are pregnant!" I heard all the nurses on speakerphone yelling and praising our pregnancy and actually felt emotions from each and every one of them coming through the phone. I almost think there were as many tears of joy happening in Dr. Miller's office as I had spewing down my face!
Over the next two weeks, I went in multiple times to assure my hormone levels were rising, and they were. Finally two weeks after we initially found out we were pregnant, we had our first ultrasound to confirm pregnancy and how many embryos took. The ultrasound technician confirmed one embryo implanted, and then we heard the heartbeat for the first time!
Our sweet girl, Elia Meadow, was born in October of 2015, four weeks early. While she had to spend a week in the NICU at the hospital, she was perfectly healthy. We were so in love with our miracle girl.
We are forever grateful for the love and support we received from Dr. Miller and the members of his team. After so many years and tears, his team made our dream a reality. There were so many times we thought we had to give in to our dream of having children, but they kept our hopes alive. Our nurse, Patty, was an absolute dream to us. I truly feel that they are just as excited as Joe and I are to have our sweet little girl. We truly believe that without the help of Dr. Miller and all his staff, we would not have our miracle baby in our arms.

Keep hope in your journey, as Dr. Miller and his team did for us. You too, can share your story one day and give hope to those who are facing infertility struggles. Thank you Dr. Miller, Patty, our nurses, and all of the staff. You have made our dreams come true with our sweet girl!
-Danielle
The Fertility Diet: Can It Boost Your Fertility?
A healthy fertility diet is one of the first things I mention when couples ask about what they can do to help achieve pregnancy. For that reason, I was interested in an article USA Today published last week discussing the fertility diet. It’s a plan based on research from the Nurses’ Health Study, one of the largest and most comprehensive studies on women’s health.
For years, I have been telling my patients to follow a diet high in protein, vegetables, fruits and iron, and low in fat and carbs. The fertility diet goes into more detail, which I certainly do not disagree with.
The study detailed steps for improving fertility through changes in diet, weight and activity for women with ovulation-induced infertility.
Here is a list of the top 10 recommendations from the fertility diet:
- Avoid trans fats. Eating trans fat raises the level of your LDL (bad) cholesterol, according to the Food and Drug Administration. It’s one of the reasons the FDA has ordered food manufacturers to phase them out.Trans fats are found in fried foods (like french fries) and in baked good (like cookies and cakes).
- Consume more unsaturated vegetable oils. Monounsaturated and polyunsaturated may help improve your blood cholesterol, according to the American Heart Association. Add more olive oil and canola oil to your diet, and try to consume healthy fats from foods like fish and avocados.
- Get more protein from vegetables. Instead of a serving of steak, consider a serving of lentils.
- Eat slow carbs. Choose whole grains, oatmeal and vegetables, which are not highly refined, over carbs like white bread and pasta, which can increase ovulatory infertility (meaning irregular ovulation or lack of ovulation).
- Make it whole milk. If you’re trying to get pregnant, a fertility diet consisting of whole-fat diary is the best choice. Opt for whole milk over skim, and enjoy a small dish of ice cream or full fat yogurt each day.
- Take a multivitamin. Folic acid (400 mcg) and vitamin B are essential. The CDC says folic acid helps prevent birth defects.
- Don’t neglect iron intake. Get plenty of iron, but not from red meat. During your fertility diet, eat vegetables high in iron, like spinach, and consider taking an iron supplement.
- Drink water. Skip the soda. Everything else (coffee, alcohol) in moderation.
- Get to a “fertility zone” weight. Being in the “fertility zone” means achieving a BMI of 20 to 24. Weighing too much or too little can affect your menstrual cycle.
- Be active. If you don’t exercise regularly, starting a workout plan could help your fertility. If you’re already active, be careful not to overdo it. According to Resolve, low body fat can affect ovulation and fertility.
The number one recommendation listed is for the use of trans fat to be drastically reduced and I must stress how important that is. I become especially concerned with a diet of excess fat and carbs when women have a hormonal imbalance related to polycystic ovary syndrome (PCOS).
I am somewhat surprised, however, with the recommendation of whole milk in the fertility diet, given the increased fat content. While it probably does not impact the normal female attempting fertility, it could have a negative effect on patients with PCOS. Dairy may even have a negative effect on endometriosis.
The PCOS patient may not only be impacted by the high fat in dairy but also by the sugar content as well. Women with PCOS have hyperinsulinemia (thus metformin is helpful). The high sugars can cause exaggeration of insulin output and long term, which can lead to weight gain. Glucose levels fall and have an impact on the menstrual cycle and egg quality.
Below is a list of foods to avoid in the fertility diet, because they can increase inflammation and may negatively impact endometriosis and subsequent fertility.
- Processed and packaged foods
- Sugar
- Gluten, white bread, and wheat
- Dairy products
- Meat (especially red and processed meats)
- Alcohol
- Fried foods
While this suggested fertility diet may not be the magic bullet couples are seeking, it is certainly a step in the right direction. Of course, every woman if different, so it is very important to talk to your physician regarding your diet.
In Good Health,
Dr. Chuck Miller
Hope for Pregnancy After C-Section: New Procedure May Help Secondary Infertility
Today's blog post is written by Michelle, a patient who was unable to get pregnant after having two c-sections and was diagnosed with an isthmocele. She traveled all the way from Houston to undergo an isthmocele repair procedure.
I was married in March of 2012 when I was 36 and my husband was 35. It was the first marriage for both of us and we did not want to waste any time starting a family. We were so excited to start our journey together and were blessed to be pregnant four months after our wedding. I took my first pregnancy test August 10, 2012, my 37th birthday, and it was positive! We both were elated. My dream to be a mom was actually happening. At first, all was going very well but by month 4 I was having extreme swelling. My doctor kept a close watch on me, but it seemed if there was anything gestational I got it! The worst was the gestational diabetes.
At my 32-week checkup my blood pressure was through the roof and at one point reached 190/115. I was immediately put in the hospital and diagnosed with preeclampsia. On my fourth day in the hospital, it appeared things were under control, until I took an extreme turn for the worse. I developed HELLP syndrome, a life-threatening liver disorder and a type of severe preeclampsia. It is characterized by Hemolysis (destruction of red blood cells), Elevated Liver enzymes (which indicate liver damage), and Low Platelet count. My liver and kidneys immediately started to shut down, so I was prepped for an emergency c- section. At the time of delivery, it was discovered I had a mild case of placenta accreta. Thankfully, my son was born very healthy considering coming so early. He was perfect, and I finally felt complete. I had dreamed of being a mommy all of my life.
Despite my complications, I knew without a doubt that I wanted more children. So, when my son was 8 months old we tried again. I got pregnant the first time we tried! I delivered my second son at 39 years old and had a great pregnancy with no complications. However, I had another C-section at 37 weeks and the doctor noted that my uterus was paper thin. He mentioned for baby #3 he would most likely deliver me at 36 weeks due to a thin uterus. Needless to say, we had our hands full with two beautiful boys that were just 18 months apart, so we knew we needed to wait a bit before trying.
After my second son was born, I noticed a difference in my cycles. They were very light and some months I didn't even have a period. I know that may not be uncommon for some women, but for me it was. Previously, I started my cycle like clockwork and was very specific in pattern every month. In addition to my irregularity, I was having extreme bloating, pain, pressure, and very light spotting that was dark in color and would last 7 to 10 days. The doctor told me that it was not unusual for your cycle to be different after having children. I went back two or three times with the same complaint and symptoms and was told I was fine. However, at Well Women checkups I was told that I had an unusual amount of cervical mucus. Well, that meant nothing to me at the time, but was key in diagnosing me later.
Fast forward to March 2016. We decided we were quite ready to try for baby #3 and naively thought it would be easy like the times before, but it was not. After 6 months of trying I went back to my OB because I was now 40 and concerned. After running some blood work, he referred me to an infertility specialist. The infertility specialist immediately told me that I was more than likely in menopause and then he proceeded to tell me that he thought I had cancer because of the amount of mucus in my cervix and uterus. I was devastated. It was 4:30 in the afternoon in the Houston Medical Center and I was all alone thinking I had cancer. A million things were running through my mind. I was thinking this just can't be happening. I immediately ran back to my OB that delivered my babies. After all, he saved my life on my first delivery and I absolutely adored him. He quickly did a biopsy and concluded I did not have cancer. Thank you, Jesus! But then we were left to figure out what was going on with the fluid in my uterus and my other symptoms. I continued to see the infertility specialist. We tried test after test and biopsy after biopsy. I even had surgery to remove "scar tissue" from my uterus. I had my tubes flushed, but nothing was helping. In April 2017 the infertility specialist had an MRI done and consulted with some other doctors. That was the first time I had ever heard the word An isthmocele is a C-section defect that occurs when the uterus does not heal correctly from the C-section incision; a portion of the two edges do not adhere. These surfaces often times become inflamed, develop scar tissue and can lead to problems with abnormal uterine bleeding, pain and infertility. I went to six doctors here in Houston, after all, this is Houston with one the best medical centers in the world. Only one of the doctors had performed the surgery one time. I was not comfortable with being patient number 2 so I set out to do my own research and that is how I found Dr. Charles Miller. I called his office and spoke with his nurse, Kate. She immediately knew what an Ismothcele was and set up a phone consultation with Dr. Miller for May 22nd. Dr. Miller was very knowledge and immediately put my mind at ease. He set my surgery for the following week for June 1st. He performed a surgery to correct my Isthmocele and also a uterine uplift procedure to keep pressure off of the newly created incision on my uterus. He was also very encouraging that I could try for baby #3 after three months post-surgery.
He concluded that the lining of my uterus measured normal and that the fluid was not present! Dr. Miller was very caring and had an excellent bedside manner. He is an extremely busy doctor, but he makes time for his patients and never makes you feel rushed. He was so positive and encouraging for me to try for baby #3. At my age, most doctors make you feel like you need to be making arrangements for a nursing home, not a baby. Now, I understand at 42 it may be more challenging, but it means a lot that he is so positive. Also, he has an amazing staff of people in his office from Theresa who performs the ultrasounds, to Kate who initially set up my consultation, to Jennifer who scheduled my surgery. I hope to follow up soon that I am pregnant!
-Michelle
Her Own View: A Patient’s Journey Through IVF- And The Results Are In...
Well... Dan and I are happy to announce, we are PREGNANT!! Dr. Miller has done it again! I took the beta test 10 days post 5 day transfer (10dp5dt), and my level was 428. To ensure you have a viable pregnancy, beta levels must double every 48 hours. I had to do a repeat blood test 13dp5dt to make sure my levels were doubling, and they were over 2600. This was exactly what we wanted to see and meant I had a viable pregnancy!
A week later, I went in for repeat blood test/ultrasound, and we saw a yolk sack and heard a heartbeat of 120 beats per minute. When the ultrasound tech was looking for the heartbeat, she had a blank face, and I was just trying to stay calm. Then I heard the heartbeat and felt such relief. I know you are thinking, “why isn’t she more excited?” I feel that after you have had losses you can never truly enjoy the moment. It’s always like “well, I hope I see a heartbeat the next time.” You only know there is a baby in there while you’re seeing it on the screen. As soon as you leave the doctor’s office, you’re anxiously awaiting the next ultrasound. But, you have to celebrate the little things so Dan and I remained cautiously optimistic…a term that perfectly describes this process.

My beta levels were also checked again and they had increased appropriately! I am experiencing pretty bad nausea (yay!), but I am trying to eat light and healthy. Thankfully, I have not experienced any bleeding, which is markedly different that my other pregnancies and makes this pregnancy feel a little different.
I am still on daily Progesterone in Oil shots (100mg), Estradiol (8mg), Lovenox 40mg, Baby Aspirin, synthetic Folic Acid and a prenatal vitamin.
I’m almost 7 weeks pregnant now, so everything is moving in the right direction. To be completely honest with you all, I am still hesitant to let myself feel completely happy due to my history of miscarriage, so I’m going to weekly therapy to help process my feelings. Every time before I go to the bathroom, I wonder if I’ll see spotting or bleeding. Fortunately, each week passes and so far we are where we need to be. My next appointment is in about a week and I will see Dr. Miller every week until I am 8 weeks at which time I will graduate to seeing my regular OB.
Dan and I hope and pray for a successful and healthy pregnancy! Wish us luck!
-Katie
Her Own View: A Patient’s Journey Through IVF- Transfer Day!
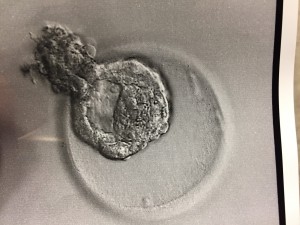
We made it!! Transfer day is finally here! I’ve spent the last few weeks prepping for the Frozen Embryo Transfer (FET). As you might have seen from the last post, preparation includes taking Progesterone in Oil (PIO) shots, Estradiol in varying dosages and other such medications. The preparation for the FET was nothing compared to the preparation for retrieval. The varying dosages can get a little tricky, but the nurses give detailed instructions so we were well-prepped for the routine. I also had to go in for bloodwork and an ultrasound to make sure my levels are good, and that the uterine lining is thick enough for the FET. Luckily, everything went according to plan, and we transferred a beautiful, hatching blastocyst this morning!
Going into the procedure, I had a lot of nervous energy, not only the day of, but the day before. I had waited SO long for this day that I was almost in disbelief that it was finally here!
This morning, I had to be at the Naperville office at 6:15AM for a 6:45AM procedure. Dan and I were taken in around 6:30AM and were both asked to put on scrubs. Dan was allowed to put his scrubs on over his clothes; however, I was asked to take off my bottoms (for obvious reasons!). The embryologist then came into the room and informed us they successfully thawed one embryo and noted that assisted hatching was not necessary since it was already hatching out of its shell! She also verified we were only transferring one. We chose to transfer only one embryo, because the possibility of having twins scares me! Also, my insurance covers IVF so I can do one transfer at a time without paying additional fees.
Once we got into the room, I was on a chair with my legs propped up (very similar to when you have your retrieval). The major difference is this time, you’re completely awake! Next, the x-ray tech came in and took some pictures of my cervix and uterus. Then Dr. Miller came in and was very jovial as usual! He said everything looked good, and proceeded to insert the catheter. This part made me feel a little crampy, but the feeling only lasted a minute so it wasn’t too bad – I would compare it to an intense pap. Then the embryologist brought our little embryo out in what looked like a really skinny straw. Dr. Miller inserted the skinny straw into the catheter, and voila, I’m pregnant (until proven otherwise)! Dan and I were able to watch everything on the x-ray screen. We couldn’t see the actual embryo since it’s microscopic, but we were able to see the air bubbles around it. It’s hard to tell in the picture below, but the embryo is the white speck in the middle of the picture. Dr. Miller reiterated that everything went as well as we could have asked for and wished us good luck!
The actual procedure only took 10 minutes and we were in the room for about 30 minutes. After I got dressed, the nurse gave us discharge instructions. I took today off from work, so I could rest and relax and will be working from home tomorrow. So far, I have stayed on the couch most of the day, but I did fold laundry and walk around a bit. I plan to take walks, but don't plan on going to the gym, because I can't have my heart rate over 140 or lift anything over 15 lbs. I was also instructed to stay on my medications until further notice. The nurse also said I might experience some bleeding. I did have some bleeding later in the morning (which is not something anyone wants to see if they are trying to get pregnant), but now, several hours later, it has mostly subsided.
Now we wait…and wait…and wait. I will take the pregnancy blood test 10 days from now. I’m excited, nervous and scared, but I think all those feelings are normal. I hope to update you all with good news in a few days. Wish us luck!
-Katie
My Journey to Motherhood: Turning a Dream into a Reality
We are honored to have Allison, a former patient of Dr. Miller's, share her story on today's blog post. 1 in 8 couples have difficulty conceiving, and as Allison writes, while there are so many people struggling, there is hope. Allison's story is an inspiration to us all.
Our journey with Dr. Miller began in June of 2015. Mike and I, high school sweethearts, had waited until later in life to get married. We were focused on our careers and, like so many others, we just assumed that once we decided to start our family, it would just happen. The first couple months of trying were no big deal. We got our hopes up a few times, but we knew that it can take healthy couples a year to conceive naturally. Well, when one year turned into two, despite trying every trick in the book and being told by our primary care doctors that there was no obvious reason why we couldn’t get pregnant, we were heartbroken. We wanted nothing more than to be parents, something that comes so easy to so many, but we just couldn’t make it happen. It was hard to admit that we needed help, but I’m so glad we did.
During our first consult with Dr. Miller he made us feel so…normal. Infertility can be such an alienating feeling, but, for once, I felt like we were going to be OK. After so much pain and hopelessness, I finally had hope. Due to irregular periods and severe cramps, Dr. Miller recommended a laparoscopic hysteroscopy to rule out endometriosis. This procedure was done in early July, and he found evidence of pelvic congestion syndrome, but no issues that should be causing infertility. We were back to square one. Still no answers, but I still had hope. We were in good hands and getting the help we needed. The plan was to proceed with 3 rounds of IUI.
After Mike and I underwent all the necessary blood tests, sperm counts, etc., it was time to start our first round of IUI in October of 2015. I was so excited to get started and optimistic that our outcome would be positive. After all, there was no obvious reason why we still hadn’t conceived! Everything went according to plan. Once I was ovulating, we went in for the insemination – everything went great. When the pregnancy test was approaching I was so excited – I just had a good feeling. I was starting to experience (what I thought) were pregnancy symptoms – tiredness, sore breasts, nausea. I thought this for sure had to be it! When my blood test revealed an HCG of 25, I was so excited! This was enough to be considered a positive pregnancy test, and we were overjoyed! However, a few days later, when we went in for repeat levels, my HCG had fallen to 4.3 – not pregnant. I was absolutely devastated. I had the next 9 months all planned out and then, just like that, it was over. I needed some time, but I was scared to throw our plan off course. When we discussed our next round of IUI with the nurses, I was scared to say that I didn’t want to try again right away. I was nervous that I would be pressured to keep going. Well, I was completely wrong. Not only were the nurses so sweet and caring, they told me to take as much time as I needed and to let them know when and if I wanted to get started again.
December 2015 and January 2016 were our second and third rounds of IUI – both unsuccessful. It was time to meet with Dr. Miller and re-evaluate. At this point in our journey, I was starting to feel discouraged. I was starting to feel like a family might not be in the cards for Mike and me. When we met with Dr. Miller, we again discussed our options. We could keep going with IUI or move on to IVF. Based on our previous experience and the much higher success rate with IVF, we decided to go forward with IVF, implanting 2 embryos.
In March, I started the IVF protocol. Birth control pills, injections (lots of injections) and ultrasounds to identify follicles. During this process, my estrogen became very high, so we were told that we could not do the transfer in the same cycle as our retrieval – another bump in the road. I was so upset having to wait another cycle, but I knew it was for the best. I had complete trust in Dr. Miller and this whole process. When we went in for the retrieval, Dr. Miller was able to obtain 18 follicles (I think…my memory is a little foggy due to the sedation). We were told this was a good number - things were starting to look up! Out of these follicles, we were able to get 10 frozen embryos. I started the IVF transfer protocol (a little different and slightly less intense with no stimulation!) and on June 6, 2016, Dr. Miller transferred two 5-day blastocyst embryos into my uterus.
On June 16, our pregnancy test was positive! And not just a little positive like last time! The subsequent days revealed climbing HCG levels and on June 28th, we had our first ultrasound of our little peanut. I had never heard a more beautiful sound in my whole life than that tiny little heartbeat of 104 beats per minute. Our second ultrasound at 7 weeks revealed a growing bean and we were discharged to OB from Dr. Miller’s office shortly thereafter.
Infertility is awful. It’s unfair and cruel. When you are struggling, just remember there are so many people out there just like you and there IS hope. Even though we’re on the other side of it now, I will never forget our journey. The ups and the downs, the good and the bad. I truly feel like Dr. Miller and his staff were there to help us every step of the way. Even during the dark times, I had complete confidence in the care and attention that was being given to us. We are forever grateful to Dr. Miller for giving us our miracle baby, Amelia Rose. Dr. Miller made our dream become a reality. I hope anyone that has stuck through this long story finds comfort in knowing that although your journey will not be easy, you are in the best possible hands with Dr. Miller.
-Allison M.
Her Own View: A Patient’s Journey Through IVF (Day 26)- Final Preparations and Waiting for Transfer Day
As you might recall from my last post, I had 30 eggs collected, and 10 made it to Preimplantation Genetic Screening (PGS). Out of those 10, five were considered genetically normal. They do know the genders of the normal embryos, but we’ve decided we don’t want to know. We have asked for the best quality embryo to be implanted during our Frozen Embryo Transfer (FET). To be honest, I’m a little surprised that we only had five come back genetically viable. As a 31-year-old, I expected a greater ratio to come back normal. Don’t get me wrong, I’m very, very grateful for having five healthy embryos. I’m also glad I did the test to up my chances of a successful pregnancy. Dr. Miller says that even in your 20s and 30s, a large percentage of eggs are genetically abnormal. Add to this, the fact that sperm can also be abnormal, it is not surprising that only 50% of the embryos were tested to be normal. He said to have five embryos tested and healthy is really very good.
This week, I went in for my FET consultation where they went over my schedule in detail. An FET is great because I now have a pretty solidified schedule for the next month and a half, so I can plan my life. The schedule was based on my ovulation, but unfortunately, I did not ovulate naturally this cycle yet. This happens sometimes because of all the stimulants in my system from my retrieval and hormones can sometimes throw off your cycle. Because of this, I was instructed to inject 3ml of Progesterone in Oil (PIO) intramuscularly to induce my period. I should have my period in the next 7-10 days and they will be able to better control my cycle once that happens. I found the PIO shot to not be as bad as people made it out to be, but again, this was my first one! I used a heating pad before/ after and massaged the contents of the shot into my bum. I was also instructed to start my Lupron injections on Friday.

After that, I start taking Estrace which helps build the lining to allow a successful implantation, Progesterone to help nourish the lining to maintain implantation and a few other things in preparation for my FET on August 28th! I do have to go in for a few more blood/ultrasound tests in the next week, but transfer day is coming up fast! I’m a little nervous that I won’t get my period, which could delay things, but it’s completely out of my hands! I’m just going to focus on self-care for the next month, and make sure I’m doing everything I can to keep myself healthy and happy!
-Katie
Her Own View: A Patient’s Journey Through IVF (Day 12-25) Adventures in Egg Retrieval
Hi everyone!
I’ve had loads of activity since the last time I updated! Since my last post, I had a third and fourth ultrasound, an egg retrieval and had my embryos shipped to the lab for genetic testing! Yes, a lot can happen in just a few days! Let me break it down…
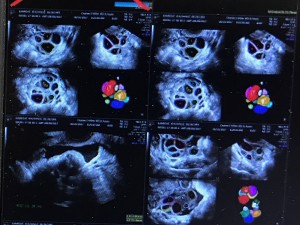
During my third ultrasound, they saw 12 follicles in my left ovary and 14 follicles in my right ovary. I’ve included a picture so you can see they were still small that day. The size is in the “mean d mm” column. For a follicle to be considered mature, they must be between 16-22mm.
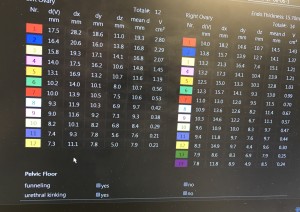
Dr. Miller requested I come back the next day after he increased my Menopur and Follistim to see if I was ready to pull the Human Chorionic Gonadotropin (HCG) trigger. The HCG trigger shot gives your follicles one last push before the egg retrieval. The shot happens exactly 35 hours before the retrieval. The next day, I had an ultrasound, and I was ready to pull the trigger at exactly 8:30 PM because I was scheduled for my egg retrieval 35 hours later at 7:30 AM. The shots during this time period were not too bad, but by the end, I was very bloated, which is a normal side effect of the medications. Yoga pants, loose tops and layers were my wardrobe staples!
So here we are, the day of the retrieval! I had to be at the office at 7 AM, for my 7:30 AM egg retrieval procedure. The staff took me in at exactly 7 AM, where they had me change into a hospital gown and gave me discharge instructions. The Anesthetist then hooked up what she needed to, and told me what to expect. The Embryologist also came in and went over the plan (egg retrieval/ freezing embryos, and Preimplantation Genetic Screening (PGS). She mentioned that there would be one update the next day, and we would not get another update until 5 days after that. The staff then took me into the procedure room where I was injected with the anesthesia. The next thing I knew, I was up and with Dan! I think the actual procedure only took 15 minutes. The first thing I heard was, “they got 30 eggs!” The staff was extremely attentive during recovery (about an hour) and Dr. Miller paid me a visit and said he was very pleased with the retrieval. After the procedure, I took it very easy and napped the rest of the day. I did take a drive with Dan that night to run an errand, which did not go well. I threw up when I got home, probably from the anesthesia and motion sickness from the car! And that is why it’s important to have a driver the day of the retrieval! The procedure was on a Sunday, and I managed to go to work on Monday, although I had to leave early. I felt uncomfortable for the next few days, but that is a normal side effect.
The next day, I received a call saying, out of the 30 eggs, 26 were mature, and 22 fertilized with ICSI (Intracytoplasmic Sperm Injection). Since I had so many eggs, Dr. Miller put me on a few medications to minimize the risk of Ovarian Hyperstimulation Syndrome (OHSS).
Often times once the retrieval takes place a transfer can be done on Day 3 or Day 5 after the embryos have matured under the care of the embryologist. This is called a fresh cycle because the embryos are “fresh out of the oven.”
However, because we chose to do the PGS testing our transfer turnaround time is a little longer. On Day 5, the lab was happy to report that I had 10 normally developed embryos that could go on to be tested for genetic normalcy. Those results should be back any day and we will then know how many viable embryos we have. After that, we will also be going through a frozen cycle. This means the embryo(s) will be thawed and then placed into their new home (aka my uterus).
To be honest, I’m enjoying this time where everything is basically out of my control. Let’s see what happens. Stay tuned!
-Katie
Her Own View: A Patient's Journey Through IVF (Days 4-11) Shots, Shots and More Shots
I have a few things to update. I started ovarian stimulation and had my first two monitoring appointments. The first appointment was 6 days ago and they took an ultrasound of the uterus to see what’s going on in there. They saw about 18 follicles on that first ultrasound, so they decided to start me on the Menopur (two vials), Follistim (150 units), Lovenox (one pre-filled injection) in addition to the Lupron. Yes, my friends, that’s four shots that I’m injecting into my belly every day! Some women want their husbands to do it, but I decided I wanted to do it myself. I think the mental aspect of taking four shots a day is a lot, and if you must coordinate with your husband to do these shots two times a day, it really adds another layer of complication--so, I stick myself! It’s kind of empowering, believe it or not!
Ok, the shots are NOT BAD! For the Menopur, I have to mix two vials of powder and one ML of solution. There are loads of tutorials on how to do this, so it’s not hard at all. This one does burn a little, but again, not too bad! Follistim is a pen, no mixing with this one. Burns a little, but again, it’s not bad. The Lovenox is by far the worst one. It burns going in. The first time I injected this one, it was PAINFUL! But, since that first injection, my expectations were set and I knew it was going to hurt. And now I’m used to it. If you make it this huge deal, then yes, it will be a huge deal. If you think of it as just part of your day, it’s no big deal. Wash your face, brush your teeth, give yourself your shot….done and done! Move on to the next thing! Also, I’ve not really felt any side effects. I’m bloated, but that could have just been the brownie I ate last night!

On the second ultrasound, they saw over 20 follicles, but all under 10mm. That means they are all small, and they need to keep stimulating me. After the appointment, they increased my Follistim to 300 units from the 150 I was originally on.
Dan and I also had to start an antibiotic to reduce the risk of infection at the time of retrieval. My next appointment is tomorrow, so I will update next week!
Thanks so much for reading!
-Katie
*Please note that each patient’s case is unique and Dr. Miller creates individual care plans for each couple based on their medical history.











