Her Own View: A Patient’s Journey Through IVF- Transfer Day!
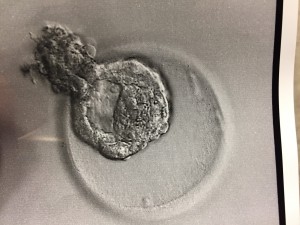
We made it!! Transfer day is finally here! I’ve spent the last few weeks prepping for the Frozen Embryo Transfer (FET). As you might have seen from the last post, preparation includes taking Progesterone in Oil (PIO) shots, Estradiol in varying dosages and other such medications. The preparation for the FET was nothing compared to the preparation for retrieval. The varying dosages can get a little tricky, but the nurses give detailed instructions so we were well-prepped for the routine. I also had to go in for bloodwork and an ultrasound to make sure my levels are good, and that the uterine lining is thick enough for the FET. Luckily, everything went according to plan, and we transferred a beautiful, hatching blastocyst this morning!
Going into the procedure, I had a lot of nervous energy, not only the day of, but the day before. I had waited SO long for this day that I was almost in disbelief that it was finally here!
This morning, I had to be at the Naperville office at 6:15AM for a 6:45AM procedure. Dan and I were taken in around 6:30AM and were both asked to put on scrubs. Dan was allowed to put his scrubs on over his clothes; however, I was asked to take off my bottoms (for obvious reasons!). The embryologist then came into the room and informed us they successfully thawed one embryo and noted that assisted hatching was not necessary since it was already hatching out of its shell! She also verified we were only transferring one. We chose to transfer only one embryo, because the possibility of having twins scares me! Also, my insurance covers IVF so I can do one transfer at a time without paying additional fees.
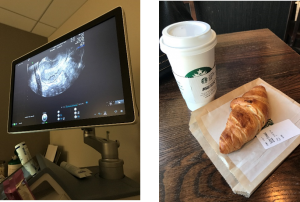
Once we got into the room, I was on a chair with my legs propped up (very similar to when you have your retrieval). The major difference is this time, you’re completely awake! Next, the x-ray tech came in and took some pictures of my cervix and uterus. Then Dr. Miller came in and was very jovial as usual! He said everything looked good, and proceeded to insert the catheter. This part made me feel a little crampy, but the feeling only lasted a minute so it wasn’t too bad – I would compare it to an intense pap. Then the embryologist brought our little embryo out in what looked like a really skinny straw. Dr. Miller inserted the skinny straw into the catheter, and voila, I’m pregnant (until proven otherwise)! Dan and I were able to watch everything on the x-ray screen. We couldn’t see the actual embryo since it’s microscopic, but we were able to see the air bubbles around it. It’s hard to tell in the picture below, but the embryo is the white speck in the middle of the picture. Dr. Miller reiterated that everything went as well as we could have asked for and wished us good luck!
The actual procedure only took 10 minutes and we were in the room for about 30 minutes. After I got dressed, the nurse gave us discharge instructions. I took today off from work, so I could rest and relax and will be working from home tomorrow. So far, I have stayed on the couch most of the day, but I did fold laundry and walk around a bit. I plan to take walks, but don't plan on going to the gym, because I can't have my heart rate over 140 or lift anything over 15 lbs. I was also instructed to stay on my medications until further notice. The nurse also said I might experience some bleeding. I did have some bleeding later in the morning (which is not something anyone wants to see if they are trying to get pregnant), but now, several hours later, it has mostly subsided.
Now we wait…and wait…and wait. I will take the pregnancy blood test 10 days from now. I’m excited, nervous and scared, but I think all those feelings are normal. I hope to update you all with good news in a few days. Wish us luck!
-Katie
My Journey to Motherhood: Turning a Dream into a Reality
We are honored to have Allison, a former patient of Dr. Miller's, share her story on today's blog post. 1 in 8 couples have difficulty conceiving, and as Allison writes, while there are so many people struggling, there is hope. Allison's story is an inspiration to us all.
Our journey with Dr. Miller began in June of 2015. Mike and I, high school sweethearts, had waited until later in life to get married. We were focused on our careers and, like so many others, we just assumed that once we decided to start our family, it would just happen. The first couple months of trying were no big deal. We got our hopes up a few times, but we knew that it can take healthy couples a year to conceive naturally. Well, when one year turned into two, despite trying every trick in the book and being told by our primary care doctors that there was no obvious reason why we couldn’t get pregnant, we were heartbroken. We wanted nothing more than to be parents, something that comes so easy to so many, but we just couldn’t make it happen. It was hard to admit that we needed help, but I’m so glad we did.
During our first consult with Dr. Miller he made us feel so…normal. Infertility can be such an alienating feeling, but, for once, I felt like we were going to be OK. After so much pain and hopelessness, I finally had hope. Due to irregular periods and severe cramps, Dr. Miller recommended a laparoscopic hysteroscopy to rule out endometriosis. This procedure was done in early July, and he found evidence of pelvic congestion syndrome, but no issues that should be causing infertility. We were back to square one. Still no answers, but I still had hope. We were in good hands and getting the help we needed. The plan was to proceed with 3 rounds of IUI.
After Mike and I underwent all the necessary blood tests, sperm counts, etc., it was time to start our first round of IUI in October of 2015. I was so excited to get started and optimistic that our outcome would be positive. After all, there was no obvious reason why we still hadn’t conceived! Everything went according to plan. Once I was ovulating, we went in for the insemination – everything went great. When the pregnancy test was approaching I was so excited – I just had a good feeling. I was starting to experience (what I thought) were pregnancy symptoms – tiredness, sore breasts, nausea. I thought this for sure had to be it! When my blood test revealed an HCG of 25, I was so excited! This was enough to be considered a positive pregnancy test, and we were overjoyed! However, a few days later, when we went in for repeat levels, my HCG had fallen to 4.3 – not pregnant. I was absolutely devastated. I had the next 9 months all planned out and then, just like that, it was over. I needed some time, but I was scared to throw our plan off course. When we discussed our next round of IUI with the nurses, I was scared to say that I didn’t want to try again right away. I was nervous that I would be pressured to keep going. Well, I was completely wrong. Not only were the nurses so sweet and caring, they told me to take as much time as I needed and to let them know when and if I wanted to get started again.
December 2015 and January 2016 were our second and third rounds of IUI – both unsuccessful. It was time to meet with Dr. Miller and re-evaluate. At this point in our journey, I was starting to feel discouraged. I was starting to feel like a family might not be in the cards for Mike and me. When we met with Dr. Miller, we again discussed our options. We could keep going with IUI or move on to IVF. Based on our previous experience and the much higher success rate with IVF, we decided to go forward with IVF, implanting 2 embryos.
In March, I started the IVF protocol. Birth control pills, injections (lots of injections) and ultrasounds to identify follicles. During this process, my estrogen became very high, so we were told that we could not do the transfer in the same cycle as our retrieval – another bump in the road. I was so upset having to wait another cycle, but I knew it was for the best. I had complete trust in Dr. Miller and this whole process. When we went in for the retrieval, Dr. Miller was able to obtain 18 follicles (I think…my memory is a little foggy due to the sedation). We were told this was a good number - things were starting to look up! Out of these follicles, we were able to get 10 frozen embryos. I started the IVF transfer protocol (a little different and slightly less intense with no stimulation!) and on June 6, 2016, Dr. Miller transferred two 5-day blastocyst embryos into my uterus.
On June 16, our pregnancy test was positive! And not just a little positive like last time! The subsequent days revealed climbing HCG levels and on June 28th, we had our first ultrasound of our little peanut. I had never heard a more beautiful sound in my whole life than that tiny little heartbeat of 104 beats per minute. Our second ultrasound at 7 weeks revealed a growing bean and we were discharged to OB from Dr. Miller’s office shortly thereafter.
Infertility is awful. It’s unfair and cruel. When you are struggling, just remember there are so many people out there just like you and there IS hope. Even though we’re on the other side of it now, I will never forget our journey. The ups and the downs, the good and the bad. I truly feel like Dr. Miller and his staff were there to help us every step of the way. Even during the dark times, I had complete confidence in the care and attention that was being given to us. We are forever grateful to Dr. Miller for giving us our miracle baby, Amelia Rose. Dr. Miller made our dream become a reality. I hope anyone that has stuck through this long story finds comfort in knowing that although your journey will not be easy, you are in the best possible hands with Dr. Miller.
-Allison M.
Her Own View: A Patient’s Journey Through IVF (Day 26)- Final Preparations and Waiting for Transfer Day
As you might recall from my last post, I had 30 eggs collected, and 10 made it to Preimplantation Genetic Screening (PGS). Out of those 10, five were considered genetically normal. They do know the genders of the normal embryos, but we’ve decided we don’t want to know. We have asked for the best quality embryo to be implanted during our Frozen Embryo Transfer (FET). To be honest, I’m a little surprised that we only had five come back genetically viable. As a 31-year-old, I expected a greater ratio to come back normal. Don’t get me wrong, I’m very, very grateful for having five healthy embryos. I’m also glad I did the test to up my chances of a successful pregnancy. Dr. Miller says that even in your 20s and 30s, a large percentage of eggs are genetically abnormal. Add to this, the fact that sperm can also be abnormal, it is not surprising that only 50% of the embryos were tested to be normal. He said to have five embryos tested and healthy is really very good.
This week, I went in for my FET consultation where they went over my schedule in detail. An FET is great because I now have a pretty solidified schedule for the next month and a half, so I can plan my life. The schedule was based on my ovulation, but unfortunately, I did not ovulate naturally this cycle yet. This happens sometimes because of all the stimulants in my system from my retrieval and hormones can sometimes throw off your cycle. Because of this, I was instructed to inject 3ml of Progesterone in Oil (PIO) intramuscularly to induce my period. I should have my period in the next 7-10 days and they will be able to better control my cycle once that happens. I found the PIO shot to not be as bad as people made it out to be, but again, this was my first one! I used a heating pad before/ after and massaged the contents of the shot into my bum. I was also instructed to start my Lupron injections on Friday.

After that, I start taking Estrace which helps build the lining to allow a successful implantation, Progesterone to help nourish the lining to maintain implantation and a few other things in preparation for my FET on August 28th! I do have to go in for a few more blood/ultrasound tests in the next week, but transfer day is coming up fast! I’m a little nervous that I won’t get my period, which could delay things, but it’s completely out of my hands! I’m just going to focus on self-care for the next month, and make sure I’m doing everything I can to keep myself healthy and happy!
-Katie
Dr. Miller Weighs In On New Medical Breakthrough: Embryo Gene Modification
It was announced this week that scientists working in a U.S. lab have used gene editing to correct a disease-causing mutation in viable human embryos. We asked Dr. Miller to weigh in on this exciting development:
I’m still excited about medicine. I remember as a young resident hearing about the first IVF pregnancy in England. Although I immediately thought of Aldous Huxley and the book “Brave New World” I knew that the technique would offer many infertile couples the opportunity to have children.
Later in the early 90s when we started to perform intracytoplasmic sperm injection (ICSI), placing the sperm directly into the egg, I was excited, as I knew that many of my infertile patients with male factor infertility would now have the opportunity of pregnancy.
Most recently, I have once again been excited about preimplantation genetic diagnosis (PGD) – an embryo biopsy technique that allows us to identify normal embryos in couples with genetic conditions so that they are able to have a normal, healthy child.
And now… I am even more excited than ever regarding the potential use of CRISPR (clustered regularly interspaced short palindromic repeats) technologies to modify genes and correct abnormal embryos. At present, when embryos are tested and are noted to be abnormal on genetic testing, they cannot be utilized. With gene modification, not only can we now make these embryos healthy and allow a healthy child to be born, but this child will no longer have the risk of passing along the abnormal gene. The potential ability to wipe out diseases such as diabetes, breast cancer and heart disease is incredible.
Certainly, this is not going to be offered overnight and moreover, one must note ethical concerns. We must be careful that this technology is not utilized to form a “super race.” Nevertheless, if utilized for the good of mankind, in my opinion, this is one of the most exciting medical breakthroughs.
In Good Health,
Dr. Miller
Additional Links:
Her Own View: A Patient’s Journey Through IVF (Day 12-25) Adventures in Egg Retrieval
Hi everyone!
I’ve had loads of activity since the last time I updated! Since my last post, I had a third and fourth ultrasound, an egg retrieval and had my embryos shipped to the lab for genetic testing! Yes, a lot can happen in just a few days! Let me break it down…
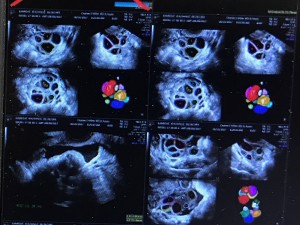
During my third ultrasound, they saw 12 follicles in my left ovary and 14 follicles in my right ovary. I’ve included a picture so you can see they were still small that day. The size is in the “mean d mm” column. For a follicle to be considered mature, they must be between 16-22mm.
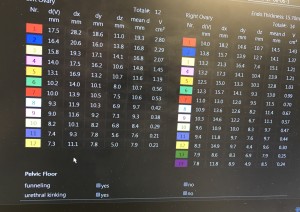
Dr. Miller requested I come back the next day after he increased my Menopur and Follistim to see if I was ready to pull the Human Chorionic Gonadotropin (HCG) trigger. The HCG trigger shot gives your follicles one last push before the egg retrieval. The shot happens exactly 35 hours before the retrieval. The next day, I had an ultrasound, and I was ready to pull the trigger at exactly 8:30 PM because I was scheduled for my egg retrieval 35 hours later at 7:30 AM. The shots during this time period were not too bad, but by the end, I was very bloated, which is a normal side effect of the medications. Yoga pants, loose tops and layers were my wardrobe staples!
So here we are, the day of the retrieval! I had to be at the office at 7 AM, for my 7:30 AM egg retrieval procedure. The staff took me in at exactly 7 AM, where they had me change into a hospital gown and gave me discharge instructions. The Anesthetist then hooked up what she needed to, and told me what to expect. The Embryologist also came in and went over the plan (egg retrieval/ freezing embryos, and Preimplantation Genetic Screening (PGS). She mentioned that there would be one update the next day, and we would not get another update until 5 days after that. The staff then took me into the procedure room where I was injected with the anesthesia. The next thing I knew, I was up and with Dan! I think the actual procedure only took 15 minutes. The first thing I heard was, “they got 30 eggs!” The staff was extremely attentive during recovery (about an hour) and Dr. Miller paid me a visit and said he was very pleased with the retrieval. After the procedure, I took it very easy and napped the rest of the day. I did take a drive with Dan that night to run an errand, which did not go well. I threw up when I got home, probably from the anesthesia and motion sickness from the car! And that is why it’s important to have a driver the day of the retrieval! The procedure was on a Sunday, and I managed to go to work on Monday, although I had to leave early. I felt uncomfortable for the next few days, but that is a normal side effect.
The next day, I received a call saying, out of the 30 eggs, 26 were mature, and 22 fertilized with ICSI (Intracytoplasmic Sperm Injection). Since I had so many eggs, Dr. Miller put me on a few medications to minimize the risk of Ovarian Hyperstimulation Syndrome (OHSS).
Often times once the retrieval takes place a transfer can be done on Day 3 or Day 5 after the embryos have matured under the care of the embryologist. This is called a fresh cycle because the embryos are “fresh out of the oven.”
However, because we chose to do the PGS testing our transfer turnaround time is a little longer. On Day 5, the lab was happy to report that I had 10 normally developed embryos that could go on to be tested for genetic normalcy. Those results should be back any day and we will then know how many viable embryos we have. After that, we will also be going through a frozen cycle. This means the embryo(s) will be thawed and then placed into their new home (aka my uterus).
To be honest, I’m enjoying this time where everything is basically out of my control. Let’s see what happens. Stay tuned!
-Katie
Her Own View: A Patient's Journey Through IVF (Days 4-11) Shots, Shots and More Shots
I have a few things to update. I started ovarian stimulation and had my first two monitoring appointments. The first appointment was 6 days ago and they took an ultrasound of the uterus to see what’s going on in there. They saw about 18 follicles on that first ultrasound, so they decided to start me on the Menopur (two vials), Follistim (150 units), Lovenox (one pre-filled injection) in addition to the Lupron. Yes, my friends, that’s four shots that I’m injecting into my belly every day! Some women want their husbands to do it, but I decided I wanted to do it myself. I think the mental aspect of taking four shots a day is a lot, and if you must coordinate with your husband to do these shots two times a day, it really adds another layer of complication--so, I stick myself! It’s kind of empowering, believe it or not!
Ok, the shots are NOT BAD! For the Menopur, I have to mix two vials of powder and one ML of solution. There are loads of tutorials on how to do this, so it’s not hard at all. This one does burn a little, but again, not too bad! Follistim is a pen, no mixing with this one. Burns a little, but again, it’s not bad. The Lovenox is by far the worst one. It burns going in. The first time I injected this one, it was PAINFUL! But, since that first injection, my expectations were set and I knew it was going to hurt. And now I’m used to it. If you make it this huge deal, then yes, it will be a huge deal. If you think of it as just part of your day, it’s no big deal. Wash your face, brush your teeth, give yourself your shot….done and done! Move on to the next thing! Also, I’ve not really felt any side effects. I’m bloated, but that could have just been the brownie I ate last night!

On the second ultrasound, they saw over 20 follicles, but all under 10mm. That means they are all small, and they need to keep stimulating me. After the appointment, they increased my Follistim to 300 units from the 150 I was originally on.
Dan and I also had to start an antibiotic to reduce the risk of infection at the time of retrieval. My next appointment is tomorrow, so I will update next week!
Thanks so much for reading!
-Katie
*Please note that each patient’s case is unique and Dr. Miller creates individual care plans for each couple based on their medical history.
Her Own View: A Patient's Journey Through IVF (Day 1-3)
Today we’re excited to share with you a new blog series about Katie, a patient of Dr. Miller’s, who has experienced difficulty conceiving. She will be sharing her fertility journey with us in her own words. Katie’s goal for journaling her journey, is that you might find comfort and strength in hearing from someone who is also going through the process as well, whether you are going through it now, or are pregnant after months (or years) of trying. Her struggle may be different, but her hopes and dreams of reaching the end goal, that bundle of joy, are the same. Although the outcome is unknown, Dr. Miller and his staff are excited to work together with Katie and her husband, Dan, as their partner and guide.
Hello Everyone!
My name is Katie and I would like to welcome you to my very first patient blog post! I’m excited to take this fertility journey with you. To give you some background, my husband, Dan and I are 31. After getting married in 2011, both Dan and I went to graduate school, which wasn’t the ideal time to start a family. Finally, at the end of 2015, we were ready to start our family. We officially started trying to conceive (TTC) in December 2015. To our surprise, we got pregnant the very first month of trying! Unfortunately, in March 2016, we lost the baby at twelve and a half weeks, a few short days after we told close family and friends. Since I had the miscarriage at home, we were not able to test for genetic abnormalities. My OB said over 50% of miscarriages happen because of genetic abnormalities, so that was most likely the reason. The entire experience was truly heartbreaking!
We were told by my OB to wait one cycle before TTC again. Since I had a D&C*, I didn’t get my first period until May 2016. In July 2016, we were pregnant again, which resulted in a chemical pregnancy* at 4.5 weeks. My OB decided to do a Recurrent Pregnancy Loss (RPL)* testing. Those tests indicated that I might have a blood clotting disorder; however, those tests were inconclusive.
My OB suggested we try again since my tests didn’t indicate any real red flags, but to take baby Aspirin for the possible blood clotting issue to be on the safe side. So we did try again, and we were pregnant again in October 2016, which resulted in another chemical pregnancy at 5 weeks. At that time, my OB agreed we should see a Reproductive Endocrinologist (RE).
After performing extensive online research, Dan and I decided to schedule a consultation with Dr. Miller in November 2016. I chose to see Dr. Miller because of his excellent reputation and success rates. Before he came in to see Dan and me, Dr. Miller reviewed my case. He said since I have an unknown reason for my recurrent losses, he would like everything tested-- from semen to genetics to blood. You name it, he’s testing it! Since I’m an HMOI patient, and Dr. Miller uses a lab outside the network, the tests had to be done through my OB.
The tests indicated that I have a MTHFR gene mutation*. This mutation does not allow synthetic folic acid to be absorbed into my body, so Dr. Miller gave me a prescription that would allow my body to absorb folic acid. I was hopeful that maybe this could be the answer.
During this time, Dr. Miller also had us do a Clomid* 50mg test cycle to see how my body would respond, but let us know that we would not be TTC just yet. We found that my progesterone was 15 Mg/Ml, lower than the 20 he likes to see with a medicated cycle. Perhaps this was another clue?
In early May 2017, we had our follow up appointment with Dr. Miller, and he talked us through all our options. He said the reasons for my recurrent losses are most likely due to a blood clotting issue or genetic abnormalities. He said we had three options:
- Clomid 100mg with Lovenox*
- IVF/ICSI* with Lovenox (50% live birth rate/ 16% chance of loss)
- IVF/ICSI with Lovenox and Preimplantation Genetic Screening (PGS)*. (70% live birth rate/ less than 5% chance of loss)
We decided to go for option 3! IVF with PGS!
So, here we are! We will do the egg retrieval in June and transfer in July! I’m currently on Lupron * 10 units, which I’ve been taking since May 23rd. Surprisingly, this injection is not bad at all. The needle is tiny and it’s relatively pain-free. I just got my period (finally!), making my cycle 32 days (very long for me as my average in 27 days). I’ll be starting my stimulation shortly here after an ultrasound in the coming days! The plan is to continue the Lupron and add Menopur* and Follistim*. The IVF nurses are really good at keeping me informed on next steps, and I also have a clear written protocol from the office.
I am cautiously excited about the next two months, but I’m not trying to get ahead of myself. I think the most important thing is to take it one step at a time, and not get too into my head about the whole process!
I’ll be updating on my IVF journey a frequently as I have new things to report!
-Katie
Katie's TCC Timeline
- 2011 – Married! Excited about life together!
- December 2015 – Removed the goalie! Let’s try to have a baby!
- March 2016 – 1st miscarriage at twelve and a half weeks. Heartbreaking. Maybe just an unfortunate fluke? Genetic abnormalities? Unknown. D&C to follow.
- July 2016 – Pregnant again! Chemical pregnancy 4.5 weeks. What’s going on here?
- August through September 2016 – Recurrent Pregnancy Loss (RPL) testing. Maybe a blood clotting issue?
- October 2016 – Pregnant again, and you guessed it…another loss at 5 weeks.
- November 2016 – Started seeing Dr. Miller. Discovered MTHFR gene mutation.
- March 2017 – Test Clomid cycle. Low progesterone.
- May 2017 – Starting IVF/ICSI with Lovenox and Preimplantation Genetic Screening (PGS). Taking Lupron 10 units since 5/23/17
- June 2017 – Got my period, waiting to go in for a baseline ultrasound and starting simulation for the retrieval!
Glossary
D&C: also known as dilation and curettage, a surgical procedure in which the cervix is opened (dilated) and a thin instrument is inserted into the uterus. This instrument is used to remove tissue from the inside of the uterus (curettage). ACOG
Chemical Pregnancy: occurs when the pregnancy hormone is elevated (i.e. beta hCG), but there are no other signs of pregnancy and it is too early to be detected via ultrasound (ivf.drcharlesmiller.com)
Recurrent Pregnancy Loss (RPL) Testing: examines genetics, infection, autoimmune testing, thrombophilia (blood clotting issues), the structure of the uterus and hormonal concerns (ivf.drcharlesmiller.com)
Clomid: Clomiphene stimulates the release of hormones needed to cause ovulation. Clomiphene therapy is typically used for 5 consecutive days early in the menstrual cycle, for 3 to 6 monthly cycles. It may take several cycles to find the right dose to stimulate ovulation. After that dose is determined, a woman will take the drug for at least 3 more cycles. If she does not become pregnant after 6 cycles, it is unlikely that further clomiphene treatment will be successful (ivf.drcharlesmiller.com)
Lovenox: Injections used to help prevent micro-clotting associated with Thrombophelia and or auto-immune deficiencies (ivf.drcharlesmiller.com)
IVF/ICSI: refers to a procedure designed to overcome infertility and produce a pregnancy as a direct result of the intervention. In general, the ovaries are stimulated by a combination of fertility medications and then one or more oocyte(s) are aspirated from ovarian follicles. These are fertilized in the laboratory (“in vitro”), after which, one or more embryo(s) are transferred into the uterine cavity. These steps occur over about a two-week interval of time, which is called an IVF cycle. (ivf.drcharlesmiller.com)
Preimplantation Genetic Screening (PGS): performed on cell(s) removed from a preimplantation embryo or a polar body from an oocyte. The goal is to identify de-novo aneuploidy in embryo(s) of couples presumed to be chromosomally normal. Theoretically, avoiding transfer of aneuploid embryos will reduce the risk of pregnancy failure and improve the probability of conceiving a viable pregnancy (ivf.drcharlesmiller.com)
Lupron: injection given below the skin, subcutaneous injection. These medications are used to enable the body to produce a higher number of quality eggs. These medications are also designed to prevent the mid-cycle hormonal surge which can result in a cancelled cycle. (ivf.drcharlesmiller.com)
Menopur: (menotropins for injection) is a prescription medicine that contains hormones. MENOPUR contains follicle stimulating hormone and luteinizing hormone activity. These hormones stimulate healthy ovaries to make eggs. (Ferring Pharmaceuticals)
Follistim: medicine that contains follicle-stimulating hormone (FSH) to help healthy ovaries to develop (mature) and release eggs; and as part of treatment programs that use special techniques (skills) to help women get pregnant by causing their ovaries to produce more mature eggs (Merck)
*Please note that each patient's case is unique and Dr. Miller creates individual care plans for each couple based on their medical history. Not all patients who have the MTHFR gene mutation will be treated with Lovenox.
Meet Dr. Kirsten Sasaki: Educating and Empowering Patients
I love being a gynecologist because I have the privilege to help women achieve better health. My goal as a doctor is to educate, inform and empower my patients so that we can work together as a team. Gynecology is a sensitive field and let’s face it, we all know how awkward an appointment and exam can be. I want women to feel comfortable discussing their concerns and issues without any judgement.
Often as the caretakers of their families, women push their own health aside. It is my job as a physician to work with my patients to ensure they prioritize their own health so they can continue to be healthy, strong and present for their families and loved ones.
Additionally, during many of my consultations, I act almost as a teacher by drawing figures and diagrams to help my patients and their family fully understand their disease and the various treatment options. So, when it comes time for treatment, the patient, her partner and her family are well-informed and ready for the next step. It is so important that patients know what to expect during and after their procedure. Listening to their worries, answering their questions and assuaging their anxieties is also a crucial part of the treatment process. I want to know what concerns them and want them to feel at ease that I have it covered. As I said, we are a team, and as a teammate I must work with my patient and guide her hand-in-hand through the process.
It’s almost ironic because not only do I consider myself a teacher of medicine, but I am also an eternal student. I have a love of learning, and practicing medicine allows me to consistently learn new things. Every day and every patient are always different and give me the opportunity to learn as I heal.
The best part of being a doctor is seeing and talking with patients I have helped. They are able to move on and enjoy their lives without having to deal with an issue that plagued them – for days, weeks or even years. Each patient has her own story, problems and goals and I love getting to know my patients in order to determine the best individual treatment plan.
I look forward to contributing more blog posts and helping women feel empowered to be an active participant in their healthcare. Reach out to us in the comments below, contact us through our website and be sure to follow our Facebook page.
Be Well,
Dr. Kirsten Sasaki
Introducing Dr. Cholkeri-Singh: Healing with Heart
When I first heard our practice was starting a blog, I couldn’t wait to write my first post. I plan to write about a variety of topics, but thought it was important for you to get to know me, understand the reason I became a physician and why helping women is so important to me.
My journey into medicine began when I was only five years old. I watched my mom struggle with a medical condition, and I desperately wanted to help fix her. As I grew older, my mom had us volunteer in shelters, and I began to enjoy servicing my community. It was then I figured out how to combine the two passions – becoming a physician would allow me to help my community and heal those with medical issues.
I specialize in gynecologic care and surgery, and I can’t imagine doing anything else. Going through my clinical rotations as a medical student, I was exposed to a variety of specialties. At first, I was drawn toward primary care because of the appeal of building long-term relationships with my patients, but at the same time, I was intrigued by surgery and the journey it takes to help cure a patient of his/her suffering.
My competing interests made it difficult for me to pick a specialty, and it wasn’t until my last medical school clinical rotation in OB/GYN that I knew for sure where I wanted to be. This field allowed for continuity of care with women while also incorporating surgical therapy for those where primary medical therapies failed. I was drawn to the subspecialty of minimally invasive gynecologic surgery and pursued a fellowship to refine my skills in surgery. This has enabled me to offer advanced surgical solutions to my patients with improved recovery times, and I am truly grateful that I am able to fulfill my childhood dream as a result.
As a physician, I understand that my patients want to feel heard and validated. They motivate me to listen, be patient and go the extra mile. I always try to be humble and treat patients to the best of my ability while constantly striving for excellence in care.
The best part of my job is receiving the smiles, the hugs and thank yous from patients whom I have helped. Whether it be providing medical counsel or performing a successful surgery to improve quality of life, their gratitude is priceless to me.
As a leading educator in the world, I am very thankful for the opportunities to teach and learn from colleagues across the globe. Not many physicians have this opportunity, so I embrace the opportunity, and I have grown significantly as a physician and human being because of it.
As Dr. Miller said in his post, we truly want this blog to be a resource for our patients and others looking for support in meeting their health goals. I’m excited to be a part of this blog and look forward to hearing from you. Reach out to us in the comments below or contact us through our website and be sure to follow our Facebook page.
Wishing you the best of health,
Dr. Cholkeri-Singh
Helping Women Navigate through Infertility and Reproductive Health Challenges
I’m excited to be writing the first post for our new blog! I say this all the time, but back in the day, when Michael Jordan and Oprah were in Chicago, I used to say I had the third best job in the city. With their absence, I guess I have the best! As a successful reproductive endocrinologist and minimally invasive gynecologic surgeon, I am fortunate enough to lecture around the world, conduct research and contribute scholarly articles to scientific journals and textbooks. However, what really motivates me is the opportunity to take care of you and help you achieve your health goals, and for many of you, help grow your family tree. That’s why this blog is for you.
I want this blog to be a resource for those seeking information about infertility treatment or gynecologic care. We will be discussing the latest in women’s health topics and sharing relevant information, research and news stories. I am so intrigued by all the medical and surgical advances we have seen since I was a medical student and look forward to sharing my thoughts as they continue to develop and expand. Not only will you hear insights from me, but also Dr. Cholkeri-Singh, Dr. Sasaki and other staff members.
I also hope to use this blog as a dialogue for my patients and anyone else who is looking for support with infertility or gynecologic care. I will write about topics you will hopefully find inspiring, offering you the strength and courage to continue to face treatments or surgery head on.
One of the best parts of being a physician is getting to know my patients and helping them resolve issues – whether it’s the resolution of pain and bleeding or finding just the right treatment plan to help a couple achieve pregnancy and fulfill their dreams of starting a family.
You’ll also hear from patients who will share their stories and journeys in hopes to show you that you are not alone in your struggle. It is a process – a very personal one, that can be long and with ups and downs -- and we are with you all the way through it.
My incredible staff will be highlighted in this blog. They are truly amazing and the backbone of my practice. Each month a staff member will be featured so you can get to know them better.
Lastly, I want to hear from you. Do you have questions about infertility, uterine fibroid treatment or endometriosis? Do you have a success story you would like to share that might give others hope? Drop us a line in the comments below or contact us through our website and be sure to follow our Facebook page.
To your health,
Dr. Miller