Do's and Don'ts During the Two-Week Wait After Embryo Transfer
Transfer Day is an exciting and hopeful point on your fertility journey, but the two-week wait that follows can be a challenging period filled with stress, anxiety and impatience. To help you make the most of this crucial time, we consulted with Monika and Mel from our amazing IVF team. They shared some important do's and don'ts to help you through the two-week wait post embryo transfer.
❌Don't Google - Trust Your Medical Team for Guidance
We know it’s tempting, but one of the most common instincts during the two-week wait is to turn to Google for answers and reassurance. However, this can lead to unnecessary stress and confusion. Remember your fertility journey is unique to you and best understood by your medical team. Rely on their expertise and guidance to ease your concerns and not Dr. Google.
✅Follow Medication Instructions
Unless instructed otherwise by your doctor, make sure to continue your medication regimen. Medications like progesterone help support embryo implantation. Consistency in following your doctor's orders is key to your success.
❌Don't Take a Pregnancy Test
It's natural to be anxious and eager to confirm a positive outcome, but taking a home pregnancy test too early can be inaccurate and potentially lead to disappointment. These tests may show a negative result because it's too soon to detect the necessary hormone levels. Or, in some cases, they might show a positive result, but the pregnancy may not continue to develop as expected. Instead, wait for the blood test, which provides more accurate and reliable results.
✅ Rest on Transfer Day, but Stay Active
While it's important to take it easy on the day of the embryo transfer, this doesn't mean you need to spend the entire two weeks in bed. Light activities such as walking can actually help boost blood flow, potentially benefiting the implantation process.
❌ Don’t Have Sexual Intercourse
To support the best conditions for the embryos to implant, refrain from sexual intercourse and orgasm during the two-week wait. This helps prevent uterine contractions that may interfere with the process.
✅ Do Delay Having a Bowel Movement
After the embryo transfer, it's wise to avoid any activities that might strain the pelvic area, including pushing during a bowel movement. Wait for about 5 hours before trying to have a bowel movement.
❌ Don't Drink Alcohol
During this critical period, it's best to maintain a healthy lifestyle, including your diet. Avoiding alcohol and focusing on a well-balanced diet is essential.
✅ Try to Relax and Manage Stress and Anxiety
Stress and anxiety are natural during the two-week wait, but managing these emotions is crucial. Consider relaxation techniques such as acupuncture, yoga, journaling or simply pampering yourself. A calm mind supports your fertility journey.
Always remember to follow the specific instructions provided by your dedicated care team. They are here to support and guide you through this journey. You're not alone, and we're here for you every step of the way.
For any concerns or questions, don't hesitate to reach out to our team. We're here to provide the care and assistance you need.
The Advanced IVF Institute Joins the CCRM Fertility Network of Clinics

Big news for our practice- the best just got better! We are pleased to announce we are now a part of the CCRM Fertility network of clinics. CCRM Fertility is a global pioneer in fertility treatment, research and science and specializes in the most advanced fertility treatments, with deep expertise in IVF, fertility testing, egg freezing, preimplantation genetic testing, third party reproduction and egg donation, achieving some of the highest Iive birth success rates in the U.S.
Dr. Miller and our dedicated and innovative team can’t wait to join forces with CCRM Fertility to provide exceptional care to our patients and give them the best opportunity for success.
Rest assured, Dr. Miller will remain as Practice Director and you will continue to receive the outstanding and personalized care you expect of us; however, now your access to top-tier medical resources has expanded to become even more innovative, efficient and accessible.
Dr. Miller had this to say: “It is an honor to join the prestigious CCRM Fertility network. Together, we are committed to our patients through innovative thought, procedures and technologies. I look forward to caring for existing patients and welcoming new patients through our doors as they face fertility and gynecologic challenges.”
We are excited to join with CCRM Fertility to bring joy to even more families! Check out the official press release below.
CCRM Fertility Broadens North American Footprint By Adding The Advanced IVF Institute to its Network
CHICAGO, Aug. 2, 2023 /PRNewswire/ -- CCRM Fertility, a global pioneer in fertility treatment, research and science, has added The Advanced IVF Institute, to its rapidly expanding fertility treatment and family-building network. Dr. Charles Miller leads two Chicago-area locations and provides cutting-edge fertility treatments, including in vitro fertilization (IVF), fertility preservation and reproductive surgery.
For more than 35 years, CCRM Fertility has helped transform lives through exceptional fertility care. CCRM Fertility's diverse, highly regarded team of physicians, research scientists, embryologists and professional staff are dedicated to helping patients achieve their dream of having a baby today, or in the future, achieving some of the highest Iive-birth success rates in the U.S. CCRM Fertility's expansive network currently serves 16 major metropolitan areas with 37 locations across the U.S. and Canada. Now, Chicagoans can have the benefit of the CCRM expertise in their own backyard.
"We are excited to welcome Dr. Miller and his team to our network, as they spearhead one of Chicago's leading IVF and surgery clinics and are recognized nationally and globally," said CCRM Fertility CEO Bob LaGalia. "Dr. Miller is an innovator in reproductive surgery and has a passion for learning new procedures, techniques and instrumentation that can positively impact patient outcomes. Dr. Miller and his experienced team will be an invaluable asset to CCRM as we collaborate to make assisted reproductive technologies more efficient and accessible for our patients."
As an internationally renowned expert in minimally invasive gynecologic surgery and in the treatment of infertility, Dr. Miller founded The Advanced IVF Institute in 2008. He is a graduate of the Honors Program in Medical Education from Northwestern University and completed his residency in obstetrics and gynecology at the University of Texas Southwestern Medical School, Parkland Memorial Hospital. Dr. Miller then earned his fellowship in reproductive endocrinology and infertility at the Hospital of the University of Pennsylvania.
Dr. Miller is a past president (2008) of the AAGL (formerly the American Association of Gynecologic Laparoscopists), the largest association of laparoscopic and hysteroscopic surgeons dedicated to the research and advancement of minimally invasive gynecologic procedures. Dr. Miller is also a past president (2011-2013) of the ISGE (International Society for Gynecologic Endoscopy).
In 2022, Dr. Miller received the AAGL esteemed distinction of Honorary Chair for his exemplary service to the AAGL and the outstanding contributions he has made in the field of reproductive medicine and minimally invasive gynecologic surgery.
Dr. Miller is the Director of Minimally Invasive Gynecologic Surgery and since 2010, Director of the Fellowship in Minimally Invasive Gynecologic Surgery Program at Advocate Lutheran General Hospital. He is the current president of the Foundation of the AAGL. He is also a faculty member of the Clinical Fellowship in Reproductive Medicine and Immunology, Rosalind Franklin University of Medicine and Science. Dr. Miller's ongoing dedication to developing young minimally invasive gynecologic surgeons earned him the AAGL's honorable John F. Steege, MD, Mentorship Award in 2018.
"It is an honor to join the prestigious CCRM Fertility network. Together, we are committed to our patients through innovative thought, procedures, and technologies," said Dr. Miller, who will continue to serve as Practice Director. "I look forward to caring for existing patients and welcoming new patients through our doors as they face fertility and gynecologic challenges."
About CCRM Fertility
CCRM Fertility is a global pioneer in fertility treatment, research and science. Founded by Dr. William Schoolcraft more than 35 years ago, CCRM Fertility specializes in the most advanced fertility treatments, with deep expertise in IVF, fertility testing, egg freezing, preimplantation genetic testing, third party reproduction and egg donation. CCRM Fertility leverages its own data and a dedicated team of in-house reproductive endocrinologists, embryologists and geneticists to deliver industry-leading outcomes. CCRM Fertility is a proud strategic partner of Unified Women's Healthcare, which is accelerating meaningful change in women's healthcare by building healthy, innovative and mission-driven businesses to meet the comprehensive needs of women across the entirety of their health journey. For more information, visit www.ccrmivf.com.
IVF Patient Journey- Karen

“I took time to educate myself about the IVF process. I started following some fertility accounts on Instagram and realized how big this community is. It’s the worst club to be a part of, but it has the best members!”
Today we are excited to introduce a new type of patient story to you. We will be sharing Karen’s journey and her efforts to become a mother. Karen had no reason to suspect she would have trouble conceiving until she tried for almost a year with no success. Now she is preparing to go through IVF and is ready to share the good, bad and the emotional with you. It is important to remember that each patient case is unique and Dr. Miller personalizes each treatment plan based on the patient’s age, medical history and test results. Here is Karen’s story:
My name is Karen and I am 38 years old, I have been married to my husband for four years and we live in Lombard with our sweet 5-year-old boxer mix, Cali. When my husband and I started trying for a family in 2021 and it wasn’t happening as quickly as I thought, I got worried. We both live a very healthy lifestyle, have clean bills of health and never thought we would have any issues trying to conceive. I had a ton of girlfriends that got pregnant very quickly, but then I also had several that went through IVF or were currently going through it. I didn’t know much about IVF because I tried not to let my mind think that would ever be an option for us. But then reality started to hit me. After eight months of no success, we decided that we needed to look into the IVF process and find a doctor.
I found Dr. Miller by doing some research on local doctors online through RE doctor websites. My friends who went through IVF all had different stories and different outcomes, with doctors all over the suburbs. My main concern was finding a clinic that didn’t make me feel like just a number. I wanted a doctor that had years of experience, would take the time to understand what we were going through and not push us through the consultation process. I also wanted to make sure there was a supportive nursing team that would be there for us during our journey. After our first meeting with Dr. Miller, I said to my husband, “Wow, this man is going to help get us our baby, I like him!”
After all the bloodwork, baseline ultrasound, HSN and semen analysis, we found out that my husband and I are both factors. Obviously my age was a huge factor and my husband had abnormal morphology, which made Dr. Miller suggest that we should go straight to IVF with ICSI (a method that involves injecting sperm directly into an egg to induce fertilization and pregnancy).
Actually hearing those words brought me to tears after we got off the call. I couldn’t believe we were going to have to go through this. A ton of questions went through my mind of why can’t I just be like everyone else, why can’t this be easy for us? I took time to educate myself about the IVF process. I started following some fertility accounts on Instagram and realized how big this community is. It’s the worst club to be a part of, but it has the best members! Finding girls that are currently going through the exact same process is a blessing. They totally know what you are going through and they feel your pains, the struggles and the wins.
Fast forward to October of 2022, and we were ready for our first round for egg retrieval. I started stims and was on a very basic protocol- menopur, follistim, ganirelix and double trigger shot. Once I got that big box of meds delivered, I was a little overwhelmed. Organizing, setting up my area where I was going to do the shots and going through the consultation with Nurse Patty, gave me the confidence that I was ready to take on the shots. I watched a ton of videos online of girls that were going through stims on Instagram to hype me up.
I had talked about the shots with my husband and showed him videos to get him ready for what I was going to be doing. I asked him (even though I knew I was going to be giving myself the shots) if he wanted to give me the shots and he said he would do them if I didn’t think I could. I let him know that he was off the hook with the stim shots, but that he would have to step up to give me the PIO shots once we got to that point in our journey.
To be honest, the shots were not that bad. Mixing and getting the shots prepped is the most hassle. I usually put on some music to sing along to as I am doing the shots to take my mind off what is going on!
I did ten days of shots and had my egg retrieval on November 3. I got six eggs! It was one more than I thought I was going to get. Results came the next day, that four matured and two fertilized with ICSI. Then we waited six more days to hear how those two did. On day 6, we received a message that only one made it to blast and a biopsy was being sent off for PGT-A testing.
We went through another long two week wait. I received the result that our only embryo was low mosaic- trisomy 1. It was heartbreaking to hear that our only embryo from our first egg retrieval had these results. We didn’t really understand what this meant, so we scheduled a follow up call with Igenomix with a genetic counselor to review the results. I am so glad we did, because after finding out what low mosaic really meant, we decided that we indeed were going to keep this embryo frozen. There might be some hope with this little embaby. After processing all this news, we knew that we had to get right back into another egg retrieval. When we first started this process, we were prepared with the possibility that we were going to have to do multiple egg retrievals based off of my test results.
At the end of November, we had our follow up consultation with Dr. Miller to review what happened and get his thoughts. He told us that this next round was going to be different and we are going to switch up the protocol now that we know what worked and what didn’t work. He gave us so much hope during that call, making sure to remind us that we are going to get our baby! Since I knew we would be starting the process again sometime in January, my husband and I just took the time to enjoy the holidays and not focus on IVF. It was a nice distraction.
Heading into round 2, I am excited and nervous. I am looking forward to seeing the end results with this retrieval since we are switching up my protocol. Even though I have been through this process once and I know what to expect, I have a feeling this path will be different and that’s ok. The main thing is that I have my support group to cheer me on, sending me positive vibes and prayers. Here we go round 2!
Stay tuned to follow Karen’s journey as she prepares for her second egg retrieval . She is excited to share her story with you and shed some light into the IVF process.
Patient Story- Lauren
“Now, I look at my daughter and have to pinch myself. I can’t believe she’s here!”
We know the holidays can be a challenging time for many of our patients. However, today we want to share Lauren’s story with you. This time last year, Lauren wondered if she would ever become a mother. Today, she has a beautiful baby girl. Unhappy with her previous clinic, Lauren came to Dr. Miller. He listened to her concerns and together they came up with a treatment plan. Another example of how important it is to advocate for yourself when it comes to your health.
Lauren writes:
My story is one of finding hope with Dr. Miller and with the wonderful staff at the Advanced IVF Institute. My husband and I had been through a lot by the time I made a teary phone call to the receptionist (or angel?) at Dr. Miller’s office. We had been years-long patients elsewhere, and had experienced four failed IUIs and two rounds of IVF yielding only one embryo and subsequent miscarriage. We were tired, sad, and wondering if becoming parents was achievable. Our previous doctor told us we would be “lucky” to end up with one child, and suggested egg donation. After researching different fertility specialists online and comparing SART statistics, I knew Dr. Miller would be the best choice for us.
When we met with Dr. Miller, he had a thorough knowledge of our history, a plan, and compassion for what we had been through. I have PCOS and thyroid disease and felt that my previous clinic did not take this into account when creating my treatment plan.
Dr. Miller took my concerns seriously and addressed them. I had concerns about insulin resistance, he investigated it and treated it. I had concerns that my previous clinic did not take my thyroid disease seriously enough and allow for appropriate monitoring, he agreed and made sure my levels were optimal before proceeding. My husband was concerned about his inconsistent fertility testing, Dr. Miller confirmed that we were dealing with an element of male factor infertility.
After our first meeting, I distinctly remember him saying, “I might not get it the first time around, but I’m confident we will get you on the right treatment plan.” Well, he did get it the first time around. Imagine our surprise and delight when on our first round with Dr. Miller we ended up with five beautiful embryos, and a pregnancy on our first transfer. He and his staff celebrated with me each week when things were going well in my early pregnancy, and by the time I “graduated” these people felt like family.
Today, we have a beautiful baby. When recovering in the hospital, my husband asked me if I thought Dr. Miller knew how much he changed our lives. When we had no hope left, he gave us everything. I think about this time last year, and not in my wildest dreams did I think I would be where I am today. I spent six years of Christmases thinking “Next year will be my year.” Now, I look at my daughter and have to pinch myself. I can’t believe she’s here!
My advice to those going through this is to live while you’re waiting. It’s tempting to throw everything you have into the process when you’re going through it. One month off from treatment to take a vacation or celebrate something special is good for your mind and body- don’t forget to nurture yourself.
Patient Story- Sheri
“We have been very blessed with great kids who seem to appreciate life, maybe because somehow, subconsciously they know that it took that extra little miracle to be here.”
Up until now, our patient stories have featured women who have recently become mothers. However, today’s submission is from Sheri, who first became a patient 20 years ago! Technology has advanced over the years, but the overarching message from Dr. Miller remains the same: “trust the process.”
My story begins many years ago (my two miracle babies are now 19 and 16)!
After years of trying to conceive, being on countless fertility drugs, endless testing and 5 years of monthly disappointing moments we decided it was time to take the next infertility step and meet Dr. Miller. My husband and I immediately felt confident he was the answer to our unexplained infertility. We left with a sense of relief. He looked us right in the eye and said “trust the process.” It was Dr. Miller’s confidence and stellar reputation that made us say “When can we start!”
The process, although long and hard at times was, by far, made less grueling and easier to face because of Dr. Miller and his staff. Every single person we encountered was kind, sympathetic, positive, caring and made us feel like they were our “infertility family”. There was one person in particular who will always stand out and be a part of my heart and that was Lynne who was at the front desk. Her smile when I walked in put me at ease instantly.
Infertility is praying endlessly. It’s sad, depressing, hard, lonely and you shed many tears. There are many roadblocks and setbacks but this journey with Dr. Miller was worth every single minute.
We were very fortunate that our first round of IVF gave us our son and our second round gave us our daughter.
Both of those IVF cycles began as multiple pregnancies but by some miracle our son and our daughter held on when we experienced vanishing embryos. It was terrifying to think we were losing the babies. I remember the moment when we thought we were miscarrying. Dr. Miller was in Europe and he called personally to ease our fears and tell me what to do to give the other baby the best chance. Grief hit hard knowing our multiples were now single pregnancies. I still think of what would have been had that not happened but take a moment to remember them and even though we never met them we love them always for what little time they were ours.
A year after our daughter was born we kept trying for more children without success. Time was not on my side because of my age. Dr. Miller saw me struggling mentally and finally gave me the strength to walk away and enjoy the 2 miracles we were blessed with.
Our son, Nick, is now 19 and studying engineering at Purdue and our daughter, Emily, is 16 and thriving in high school. Every moment of their lives has been better than the next. We have been very blessed with great kids who seem to appreciate life, maybe because somehow, subconsciously they know that it took that extra little miracle to be here.
To all the patients present and future…I pray for you, I wish you peace always and I hope your dreams come true. You deserve to be parents!
Patient Story- Breda
“Not everyone will understand IVF or be able to relate, so it’s important to surround yourself with support. More people than you realize struggle with infertility.”
Today’s patient story is from Breda. After not finding success or feeling comfortable at another fertility clinic, Breda came to us. We are all glad she did! Dr. Miller was able to diagnose her with endometriosis and after surgery and IVF, she was able to get pregnant. Breda is due in January!
Breda writes:
I met my husband later in life and we got married when I was 38. I was and still am wary of the stigma of older mothers, even though being older is accepted. I’ve always wanted a family and we started trying right away, but I had three miscarriages in a year and a half. I was at a different fertility clinic for a year, but didn’t feel comfortable there. My husband’s colleague recommended we see Dr. Miller and what a difference!
We first met online during COVID and Dr. Miller told us, “You’ll be a mother, kiddo.” He was so kind, didn’t rush us, and he explained everything. He learned I was an English teacher and told me a story that put me at ease. He never stopped his storytelling, and I welcomed his personable demeanor after some bad experiences at the previous clinic. Dr. Miller found issues that the previous doctor did not, including endometriosis.
After a biopsy, Dr. Miller found abnormalities in my uterus and I was diagnosed with Level 1 endometriosis. During surgery, he removed five spots on my uterus. I also had the Endometrial Receptivity Assay biopsy to determine the receptivity of the uterus to implantation. Soon after, we had an egg retrieval and two transfers.
Throughout this process, Dr. Miller and his staff explained everything so thoroughly and never seemed irritated or disinterested when I had questions. I also got to know Dr. Miller and the nurses because they talked to me during appointments. I always felt people cared and were invested in our success. I felt so secure going into our procedures and never felt anxiety or stress visiting the office.
Even though our first transfer failed, a second embryo implanted and I will never forget that experience. Dr. Miller, Courtney, and Melody were present for the transfer, and made me feel so comfortable. Dr. Miller even told us a funny story about meeting an actor from Will & Grace. While we waited after the transfer, my husband and I held hands and prayed, and we also talked about how wonderful it would be if it worked. Many times, we dreamed of finishing our nursery and being able to move forward with our plan. The transfer worked, and our baby is due January 8, 3.5 years after we began IVF and what seems like a million doctor appointments.
I was very nervous the first 12 weeks of my pregnancy and braced myself for bad news, but at every ultrasound Courtney reassured me with her positivity. We are so grateful for everyone at the Naperville office.
It took until I was about 20 weeks pregnant for me to relax and realize we’re finally going to be parents! I’ve cried many happy tears for a change! Not everyone will understand IVF or be able to relate, so it’s important to surround yourself with support. More people than you realize struggle with infertility. Meditation and journaling are helpful (as well as long walks with our dog, my first baby). Finally, never stop hoping and praying, even if you’re an older mother!
Patient Story- Molly
“We have been so blessed that I know all the pain and suffering we endured was worth it.”
We’re featuring Molly’s story today! Molly’s story is unique because she was diagnosed with unexplained infertility. This is a tricky diagnosis, because even after testing a cause cannot be determined. When this is the case, there is a lot of trial and error in order to achieve pregnancy. But as Dr. Miller always says: “Trust the process.” That’s just what Molly did and now she has two beautiful sons. Read her story below.
I first became a patient of Dr. Miller’s in 2012 when I had a myomectomy, a surgical procedure to remove uterine fibroids. After getting married and trying for several months to get pregnant, a co-worker suggested I see Dr. Miller, but this time as a fertility specialist. At our first appointment, Dr. Miller ordered blood work and a hysterosonogram which is an ultrasound exam that provides images of the inside of the uterus to help diagnose the cause of abnormal vaginal bleeding. However, everything came back fine. I was told I had unexplained fertility. This wasn’t the news I wanted to hear! It would have been easier to have a specific reason for why I could not get pregnant.
I was put on medication for thyroid and prolactin issues. After a month on the medication, it was advised we try an IUI. We failed all three attempts. Dr. Miller said IVF would need to be our next step. Soon after, my retrieval resulted in 26 eggs! My husband and I were so excited, our dream of having a baby was one step closer.
However, we were unable to do a fresh transfer at that time because I was borderline for Ovarian Hyperstimulation Syndrome (OHSS). This occurs when a woman’s ovaries swell and leak fluid into the body. This condition is temporary and occurs in less than 5% of women who receive fertility treatments. Instead, we ended up freezing 8 embryos. About two months later one embryo was successfully transferred. It was a strange feeling, because I was so happy and terrified at the same time.
After graduating from Dr. Miller’s office, my OB/GYN monitored me closely and that little embryo was born at 34 weeks gestation. Again, I was happy and terrified at the same time. Thankfully our little boy was healthy and strong.
After our son turned 18 months, we decided to start the process to have another child. We decided to follow the same protocol as before and do a transfer in three months. Unfortunately, it failed. After meeting with Dr. Miller again, he advised us to do a trial cycle with an Endometrial Biopsy (EMB). An EMB tests whether the uterine lining is preparing itself adequately for implantation of the embryo. If the lining is out of phase, it can prevent implantation from occurring or result in an early miscarriage. Because the results of my EMB were abnormal, I was treated with progesterone. The following month we had another transfer and it was successful! We welcomed our second baby boy this June./p>
Our two little boys are thriving! We are so happy we found Dr. Miller and are so grateful for everyone in the office as well as Dr. Deutch who did our last transfer. Our advice to other couples going through infertility is to know that you are strong, brave and deserve to be parents. Don’t ever give up! We have been so blessed that I know all the pain and suffering we endured was worth it.
Patient Story- Julia
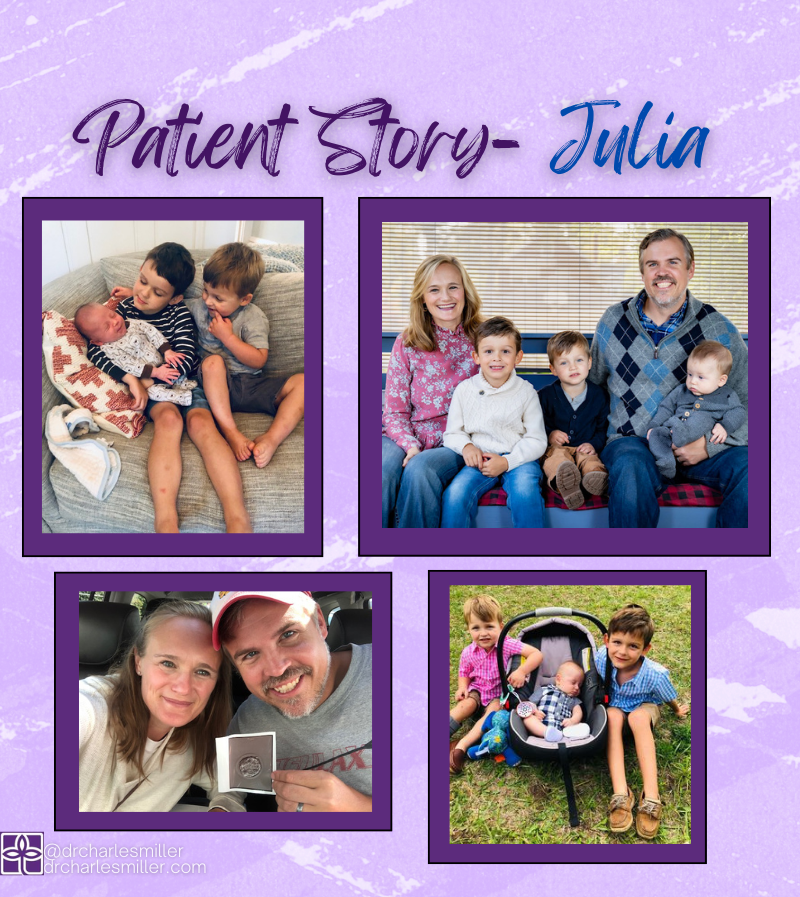
“This is why you keep fighting; so that you can have peace. Whatever outcome will bring you peace, that is what you fight for.”
Julia is a patient that our office has known for quite some time. She recently welcomed her third baby boy and we have enjoyed getting updates and pictures throughout the years. A seasoned IVF veteran, Julia has been through it all and yet she is incredibly candid about her experience. This openness has led her to volunteer to answer calls for the Resolve support line twice a month. While there aren’t many calls, she is so grateful when she gets to speak to someone and give them some hope. We are so grateful that Julia has shared her story.
She writes:
The other day, I took my two older boys to the fire station open house. It was absolutely packed, it seemed like everyone from our town was there. I looked around at all of the children, moms, dads, siblings, grandparents, etc. and had a moment of self-doubt.
“I don’t belong here,” I thought to myself. “This event is for families.”
As if on cue, my middle son reached up to hold my hand, and my older son ran ahead and called out for me. “MOM! This way, follow me!”
I was instantly brought back to reality, my feelings of insecurity disappearing and belonging restored. I am a mom (of three boys!), and I DO belong at family events, school drop-off, parent-tot classes, parks and baby pools, and in the club that is Parenthood.
The lingering grief and pain of infertility can rear its ugly head at the strangest moments, like it did that Saturday morning. I remember the feeling of fear so well; the fear that I would never become a mom. I know all too well how painful the treatments and the unknowns are as I fought long and hard for my boys. However, I also know the peace that comes from a dream achieved. I want to instill hope in anyone who has that fear and pain, who is in the throes of fertility treatment, who is struggling with self-doubt and the unknown.
I have three beautiful and healthy boys. They are almost perfectly spaced apart; 2.5 years. From the outside looking in, we are a very typical family. And in most senses, that is correct – except for how our family was created.
We waited four years for our first son. I worked for one year with my ob-gyn and Clomid. I then had six stimulated rounds with my first fertility specialist and one miscarriage. When I met Dr. Miller, I had two more failed IVF rounds before we chose to use a donor egg. I had a polyp removal surgery. I did three trial cycles to determine the optimal window for an embryo transfer. We lost our first donor due to poor response to stimulation while I was on hormones alongside her. With our second donor, my first transfer was a blighted ovum that ended in two separate D&C surgeries. After extensive blood work, I was diagnosed with MTHFR, a genetic blood-clotting disorder that can affect implantation.
On November 9, 2016, my 13th cycle, I became pregnant with my first son.
Charlie was cycle 13. James was cycle 15. John was cycle 16.
I share the details of my journey not to overwhelm you, but to give you strength. Maybe your journey will be shorter than mine. Maybe it will be longer. It often felt daunting, hopeless at times, and never-ending. I remember the receptionist at Dr. Miller’s office pulled out my file. It looked like several copies of the Yellow Pages stacked on top of each other. During one of my meetings with Dr. Miller, he put his hand on top of that file and said, “Julia. We haven’t been through this much, for you to not get pregnant. I WILL get you pregnant.” I trusted him and pushed forward despite the fear and pain.
This is why you keep fighting; so that you can have peace. Whatever outcome will bring you peace, that is what you fight for. And you will know when that time comes. People ask me how I did it. They want to know how I managed the appointments and driving, the shots and tests, the physical side effects and emotional trauma, the disappointment and the grief.
I tell them the truth; you just do it. You have to keep going so that you can have your peace.
I promise that the grief and fear will fade with time. It might make an appearance here and there after you have achieved your dream, but that is just a little bit of PTSD from the journey. It will fade. You will hold your little miracle, you will walk with your child at the fire station open house, or into that parent-tot gym class, or to the first day of preschool, or story hour at the library and you will belong. You will feel peace.
Believe in Dr. Miller. Believe in his nurses, the ultrasound techs, the phlebotomist, his entire staff. Throw in some prayers, push forward, and wait for your time to come.
Patient Story- Rachael

“Our plan was always to have a baby, but our path certainly wasn’t a straight line.”
Our next patient story is from Rachael. Rachael’s journey to motherhood has not been an easy one. After undergoing several unsuccessful rounds of IVF, Dr. Miller advised Rachel to consider using an egg donor. In her story, Rachel describes the process she and her husband went through to choose an egg donor and what advice they would give to others in her situation. Rachael’s story has a happy ending- she is now pregnant and due with a baby boy in February!
Rachael writes:
To say that our journey was a difficult one is an understatement.
I was 34 years old when we wanted to start our family. After six months of trying on our own, we met with Dr. Miller. Testing and medication followed, and we eventually discovered – after finding out I had a diminished ovarian reserve, as well as confirming that I had a unicornuate uterus – that IVF was a route we needed to take. We diligently went to work ordering medication, setting up appointments, and saying so many prayers. Unfortunately, our first round failed. We just kept thinking, “This is it!” only to find ourselves back at square one.
When I met with Dr. Miller for our follow-up consult, he had another plan to try again. Upon leaving our meeting, he told me, “Stick with me, Rach! Rome wasn’t built in a day.” Knowing this was true, and knowing we had faith in our doctor, we trudged ahead and kept going. What followed were an additional five rounds (some stopped before retrieval), further testing and added medication, laparoscopic surgery, and the need to put on more weight in hopes that it would help my egg quality.
After several additional rounds of IVF and additional embryos from said rounds that didn’t take, our insurance plan was running out of options for us to keep moving forward. Dr. Miller advised us not to do the egg retrieval with my own eggs at that point and suggested turning to an egg donor. We were absolutely heartbroken. We knew that this was a real possibility, but the news was hard to take in. We were at the end of stimulation injections, and my body just wasn’t cooperating (which had happened during another of our previous cycles). Knowing my track record, Dr. Miller was concerned that this round would not work and then we’d really be out of options with my insurance. We converted the round to an IUI, but it didn’t take. A month later we transferred the one frozen embryo we had (insurance would still cover that), but we were left with a negative result.
We were angry, frustrated, and beyond depressed. We knew it was no one’s fault (I had to keep reminding myself that I did nothing wrong), but we couldn’t understand why it was happening. We did absolutely everything we possibly could to have a positive outcome, but were left with nothing but grief. You know everyone means well when they offer their condolences, but there are times when IVF is an incredibly isolating experience.
A few months later, we met with Dr. Miller again to discuss using an egg donor. He answered all our questions and felt optimistic about this new plan. When we were ready, we contacted an agency to get information. Later that fall, we chose our egg donor and started to feel more optimistic ourselves. Our donor went through the testing process and started some medication. We had psychological evaluations to make sure that everyone was in the right state of mind to go through this process, and we met with a lawyer to go through the contingencies of everything.
Our donor finally had her egg retrieval in February; we received 48 eggs (which was incredible!), and out of the 48, we had 17 embryos to freeze. We couldn’t quite sync up cycles, so we worked toward an April transfer, but then that got canceled due to me catching COVID-19. We were finally able to complete our transfer in May, and at the end of the month we received our first positive pregnancy test! I’m due in early February with a boy and am currently 18 weeks along (for a frame of reference, I am now 39 years old).
Moving forward, we have 16 embryos at our disposal. Besides some days where I didn’t feel great in the first trimester, my energy has bounced back in the second trimester and I feel pretty good! We’re really looking forward to the future and still cannot believe that we’re on the other side after years of wondering “what if?”
It was a long, difficult four-and-a-half years to get to this point. There were so many tears, early morning appointments, and hours upon hours of frustrating phone calls with insurance and pharmaceutical companies. There were so many pregnancy announcements by friends and family. There were so many times when we felt raw, numb, and alone. But on the other hand, we had hope. We had a strong support system, and we had a caring doctor who genuinely wanted the best for us. Dr. Miller’s staff was so kind and offered me hugs on more than one occasion when we received bad news. We learned to give into the unknown (something difficult for us teachers to do) and trust that we were doing everything we could.
If I can offer advice, I’d stress the importance of learning to pivot. Our plan was always to have a baby, but our path certainly wasn’t a straight line. We had to adjust the details of our dream, but that doesn’t mean that we’ll be any less of parents than we would have if things had worked with my genetics. Our dream could still be a reality, but adjustments were needed. Keep the end goal in mind: if it’s to have a child, understand that what that means might look different than what you anticipated when you started the journey.
If you find yourself in need of an egg donor (or sperm donor, if that’s the issue), I’d encourage you to take your time and go through the process when you’re ready. Don’t try to look for yourself in the pool of applicants; you won’t be there, and that’s okay. When we first got information from the egg donor agency, they encouraged us to not pay as much attention to pictures, but to focus on the information: we examined their health history and that of their relatives; we listened to their reasons for being a donor; we screened applications for the possibility of twins and triplets (given my unicornuate uterus, multiple births at one time was not considered a viable option); we also poured over their previous donor cycles to see what kind of success they had.
In the end, we chose someone who looked happy. She genuinely wanted to help other people conceive and assisted others in that goal already. The agency (and Dr. Miller’s office) couldn’t say enough good things about her, which was really reassuring. Besides matching my ethnicity, she does not look like me, but I’m keeping in mind that our boy very well may look more like my husband than the donor. If he doesn’t, that’s okay, too. This was something I had to learn to get comfortable with before we officially went through the donation process.
There are times when I look back at the last few years and the pain comes crashing back, and I’d be lying if I said it was easy to move on from my genetics. However, at the end of the day, the goal is to have a baby, and I learned that it is still possible if my genetics are no longer an option. This could be a path for you, too.
We would also encourage you to let people in and have a support network. My husband and I did not always want to talk about our struggles, but knowing we could speak with family and friends was helpful (and there are other support groups if you aren’t getting the support you need from those around you, too). Even though most of the people you know might not “get” the struggle you’re going through, it’s important to remember how many people are in your corner. You’re going to feel alone. You’re not.
Keep the faith. We’re rooting for you!
Patient Story- Courtney

“Keep going even when it feels like you can’t… The little victories will give you strength.”
Today’s patient story is from Courtney. Courtney discovered she had endometriosis when she and her husband were not able to conceive naturally after several months of trying. After undergoing surgery with Dr. Miller, she was able to get pregnant via IVF and just welcomed a baby boy only three weeks ago! Congratulations Courtney!
Courtney writes:
My husband and I began trying to conceive in late 2017. While at my yearly gyno appointment in May 2018, I mentioned we were trying to conceive. I was told to track ovulation with an app and/or pee sticks and go from there. My period had always been like clockwork and I learned that my ovulation was too. I maybe had heavier/more painful periods but nothing that ibuprofen and a heating pad couldn’t fix. My gynecologist did an internal ultrasound and noticed that one ovary was dense, leading her to believe that I might not ovulate on that side, however my pee sticks indicated that I did.
We ended up getting pregnant on our own in the summer of 2019, but that ended in a miscarriage (D&C) as there was nothing in the sac. I then had the dye test to see if my tubes were blocked and they were not. I also did 3 rounds of clomid with no pregnancy. This was the end of the road with my regular gynecologist as she couldn’t help me any further.
I then went to another gynecologist in my hometown to move onto IUIs. He did a natural IUI with no luck. Then we tried a medicated (clomid) IUI with no luck either. During this process, he did an internal ultrasound and that’s when I first learned I possibly had endometriosis. He referred me to Dr Miller.
I had laparoscopic surgery with Dr. Miller in Feb 2021 for endometriosis. We decided to try surgery before an egg retrieval, because Dr. Miller thought he could clean me out and then we could try to conceive naturally or with clomid as he didn’t think the endometriosis was as bad as it turned out to be. However, during surgery he found stage 4 endometriosis on my ovaries and appendix. He removed my appendix and did what he could on my ovaries in order to preserve them for IVF.
After my surgery, Dr Miller said that the endometriosis had been there for quite awhile because the cysts were so fixed to my ovaries. He said he did what he could to minimize the cysts but he couldn’t get rid of them fully because that would ruin good ovarian tissue for IVF. After I’m done having kids, I can have another surgery to fully clean me out.
It was invaluable to have Dr. Miller as my surgeon and fertility specialist. The entire time he was focused on the goal at hand- to have kids. I felt comfortable during the process that he knew what to do during surgery to make it possible for me to have kids.
After surgery, we started preparing for IVF and I had my egg retrieval in July 2021. We ended up with 4 well graded, untested embryos after retrieval. My first FET (frozen embryo transfer) was in September 2021 and unfortunately ended in a chemical pregnancy. Shortly thereafter, we did another transfer and I gave birth to my son, Leo, on August 11.
Going through infertility takes a toll on you emotionally and physically. Here are a few pieces of advice I would give to other women dealing with infertility.
- Keep going even when it feels like you can’t do/go anymore. The little victories will give you strength. For example, the recovery from retrieval was brutal for me, but when we found out we got 4 embryos, I felt like I could do it all over again.
- Ask for help and allow help from others. I am the most organized person out there but I had to have my husband take the reins on the meds because it was all too much for me. I never prepared, mixed, set up, or gave myself one shot!
- Don’t change your lifestyle. Dr Miller never once told me what to eat, drink, do, or not do. Working out was limited with retrieval and FET, but that was the extent of it.
- Take the month off and go on vacation. Dr Miller wrote in my message on the portal that this was a must! You have to continue to live your life as best as possible!
